Back Pain Breakthrough: Are Your Pedicle Screws Missing the Mark?
"New research suggests traditional spinal fusion techniques might be overlooking key areas for optimal bone density and fixation strength. Discover how alternative placements could revolutionize back pain treatment."
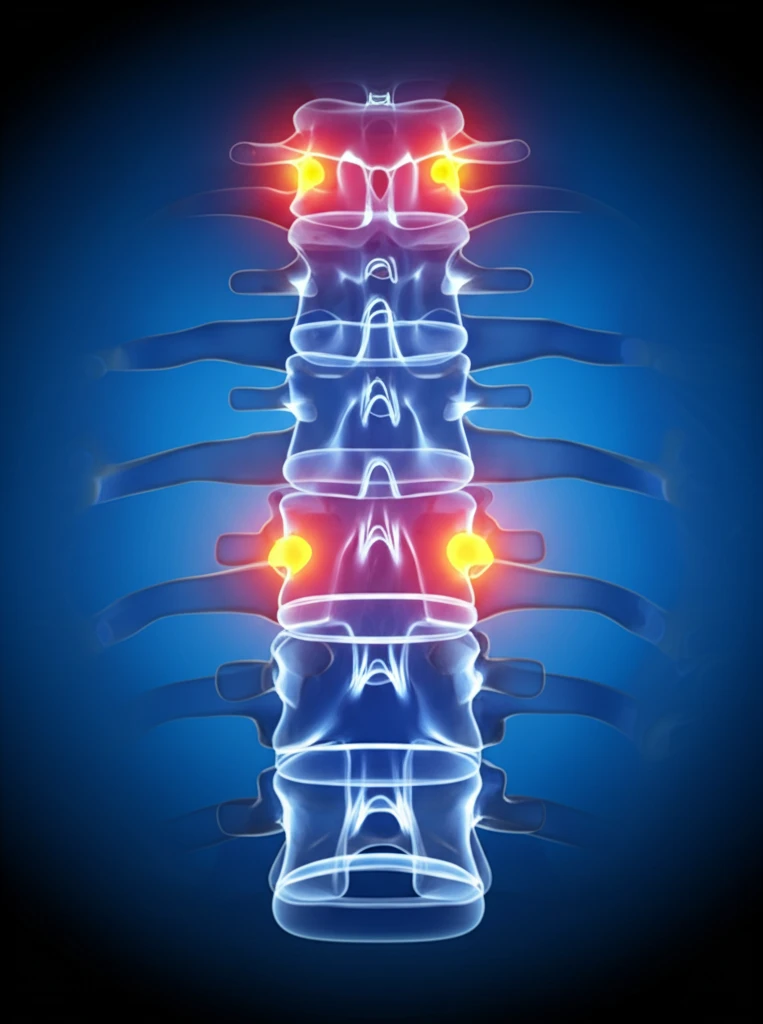
Chronic back pain is a widespread issue, and for many, spinal fusion surgery offers a beacon of hope. A critical factor in the success of these procedures is the strength of the bone where implants are anchored. Traditionally, surgeons have relied on pedicle screws, assuming the pedicles—small, paired bony structures that connect the vertebral body to the posterior elements—offer the best fixation points. But what if this assumption is wrong?
A groundbreaking study is challenging this long-held belief, suggesting that pedicles might not be the densest regions of the lumbar vertebrae. This could have significant implications for how spinal fusion surgeries are performed, especially for individuals with osteoporosis or other conditions that compromise bone quality. The research opens the door to exploring alternative sites that could provide more secure and lasting fixation, ultimately reducing the risk of implant failure and the need for revision surgeries.
The quest for more effective spinal fusion techniques is particularly crucial given the aging population and the increasing prevalence of osteoporosis. As more individuals undergo these procedures, understanding the nuances of bone density within the vertebrae becomes paramount. This article delves into the findings of this study and what it means for the future of back pain treatment.
The Bone Density Puzzle: Rethinking Spinal Fusion
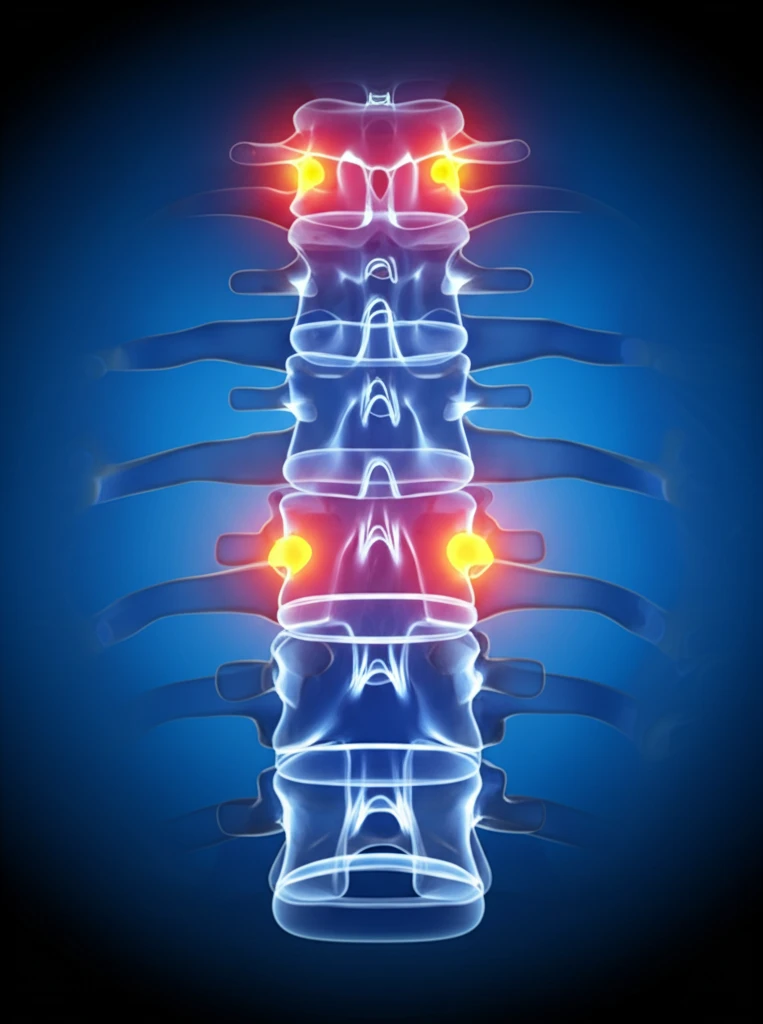
The study, a detailed examination of cadaveric lumbar vertebrae, employed computed tomography (CT) imaging to assess bone mineral density (BMD) across various anatomical subregions. Researchers digitally isolated the spine and meticulously segmented each vertebra into seven distinct regions: the vertebral body, pedicles, transverse processes, lamina, superior articular processes, inferior articular processes, and spinous process. By converting Hounsfield units (HU), a measure of radiodensity obtained from CT scans, into BMD values, the team was able to map the density landscape of each vertebra.
- The lamina and inferior articular processes have the highest bone mineral density in the lumbar vertebrae.
- The vertebral body has the lowest bone mineral density.
- Pedicles have moderate bone mineral density, lower than the lamina and inferior articular processes.
- These findings challenge the traditional focus on pedicles as the primary fixation point in spinal fusion surgery.
The Future of Spinal Fusion: A Shift in Perspective
This research signals a potential paradigm shift in how we approach spinal fusion surgery. By recognizing the variations in bone density within the vertebrae and exploring alternative fixation sites, surgeons can potentially improve outcomes, reduce complications, and enhance the quality of life for countless individuals suffering from chronic back pain. Further research is needed to validate these findings and refine surgical techniques, but the future of spinal fusion looks promising, with a renewed focus on personalized approaches and optimized implant placement.
