Aortic Thrombosis After Chemo? How a Minimally Invasive Procedure Saved the Day
"Discover how endovascular treatment offers a beacon of hope for high-risk patients facing acute aortic thrombosis following cisplatin-based chemotherapy."
Cisplatin-based chemotherapy, while effective against cancer, carries a significant risk of thromboembolic events. Acute thrombosis of the aorta, a rare but serious complication, demands swift and effective management. This article explores a case where a patient developed this condition following chemotherapy for gastric cancer.
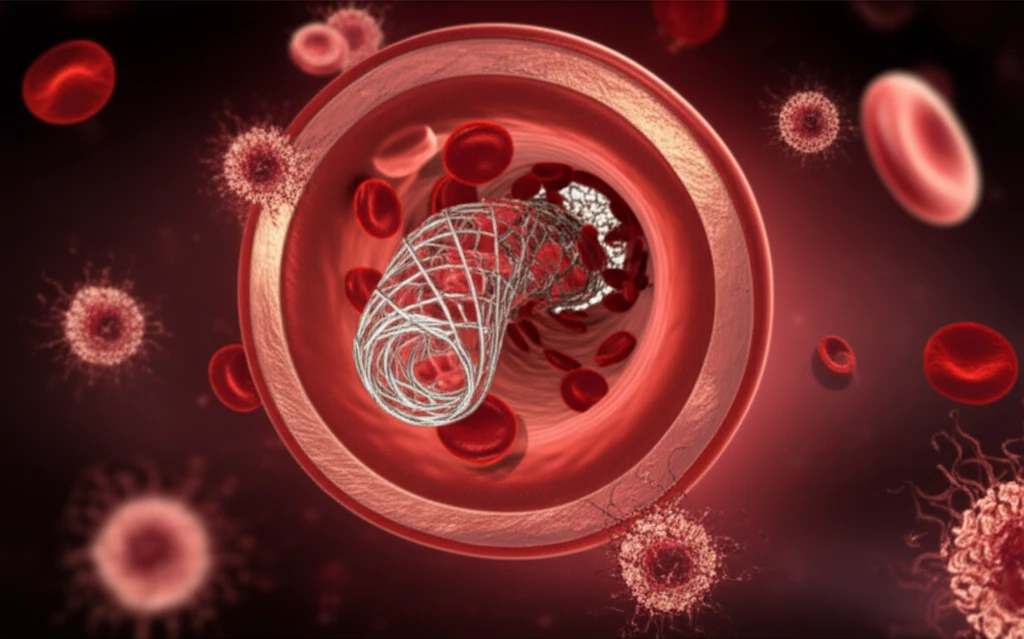
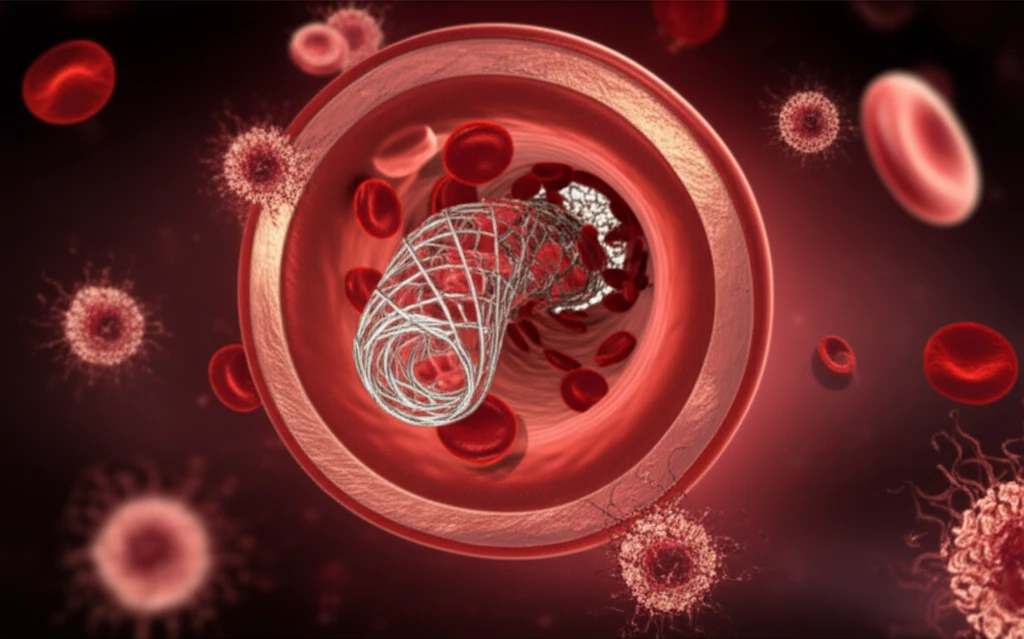
Traditional treatments for aortic thrombosis include thrombolysis, anticoagulation, and surgical removal. However, these approaches may not always be suitable for high-risk patients, especially those with underlying malignancies or those needing further surgery. Endovascular treatment offers a less invasive alternative, potentially reducing the risks associated with open surgery.
This article delves into a specific case where endovascular treatment, combining Fogarty thrombectomy and stent graft exclusion, was successfully used to manage acute abdominal aortic thrombosis in a patient who had undergone cisplatin-based chemotherapy.
The Case: Acute Aortic Thrombosis Following Chemotherapy
A 75-year-old male undergoing preoperative cisplatin-based chemotherapy for advanced gastric cancer experienced severe abdominal pain and calf claudication just three days after treatment. A multidetector computed tomography (MDCT) scan revealed a floating mass in the infrarenal abdominal aorta, a previously unseen condition.
- Fogarty Thrombectomy: A catheter with a balloon is inserted into the artery to remove the thrombus (blood clot).
- Stent Graft Exclusion: A stent graft is placed to cover the damaged area of the aorta, preventing further clot formation.
Endovascular Treatment: A Promising Alternative
While surgical removal remains a standard treatment for aortic thrombosis, endovascular treatment offers a valuable alternative, especially for high-risk patients. It provides a less invasive approach, potentially reducing complications and improving recovery times.
The combination of Fogarty thrombectomy and stent graft exclusion appears to be a safe and effective strategy for managing acute aortic thrombosis following chemotherapy. However, further research is needed to establish clear guidelines for postoperative anticoagulation and long-term management.
This case highlights the potential of endovascular treatment as a reliable and less invasive option for patients with acute aortic thrombosis, particularly those with underlying conditions that make open surgery a higher risk.
