Aortic Dissection Breakthrough: How a Minimally Invasive Procedure Saved a Life
"Learn how a novel percutaneous approach restored blood flow to critical organs in a patient with a life-threatening aortic dissection."
Aortic dissection, a tear in the inner layer of the aorta, is a critical condition demanding rapid intervention. Untreated, it carries a high mortality rate, with approximately 50% of patients dying within 48 hours of onset. The Stanford Type A dissection, specifically, involves the ascending aorta and necessitates prompt management to prevent life-threatening complications.
Traditionally, surgery has been the primary treatment for Stanford Type A aortic dissections. However, when complications arise, such as compromised blood flow to vital organs, pre-surgical interventions become necessary. These complications increase the risk associated with surgery, prompting the exploration of less invasive approaches.
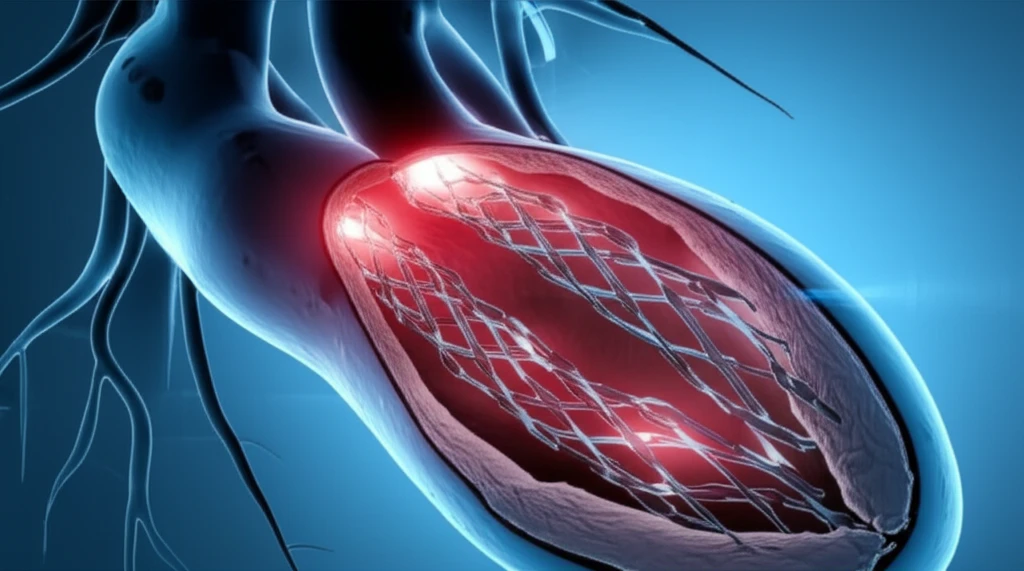
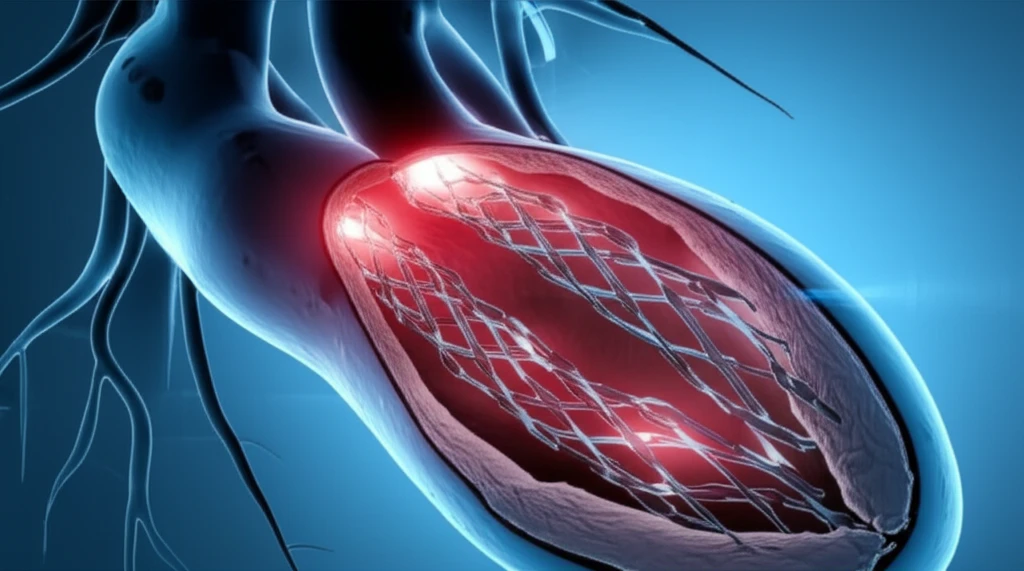
This article delves into a compelling case where a patient with a Stanford Type A aortic dissection experienced a blockage of blood flow to the lower abdomen and kidneys. To restore circulation and stabilize the patient for surgery, doctors employed a percutaneous (through the skin) approach involving fenestration (creating a hole) and stent placement. This case highlights the potential of minimally invasive techniques in managing complex aortic dissections.
The Case: Restoring Blood Flow with Innovation
A 61-year-old woman presented to the emergency room with severe back pain and lower extremity weakness, classic signs of aortic dissection. Her medical history included hypertension, and initial examination revealed absent pulses in her legs. A CT scan confirmed a Stanford Type A aortic dissection with complete blockage of the aorta below the kidneys.
- Femoral Access: Catheters were inserted through the femoral arteries in the groin.
- Fenestration: A special needle was used to create a channel (fenestration) through the dissection flap, connecting the false lumen (the space created by the dissection) to the true lumen.
- Stenting: A stent (a small mesh tube) was deployed to keep the fenestration open and support the true lumen, ensuring adequate blood flow.
A Promising Alternative
This case demonstrates the potential of percutaneous fenestration and stenting as a valuable tool in managing complex aortic dissections, especially when critical organ ischemia is present. By restoring blood flow prior to surgery, this approach can improve patient outcomes and reduce the risk of complications.
While surgery remains the definitive treatment for Stanford Type A aortic dissection, minimally invasive techniques offer a crucial bridge to surgery in patients with compromised organ perfusion. These procedures can stabilize patients, improve their overall condition, and increase the likelihood of a successful surgical outcome.
Further research and experience will refine the techniques and identify the ideal candidates for percutaneous intervention in aortic dissection. However, this case provides compelling evidence that these approaches can be life-saving in select patients.
