AML Breakthrough: Can a New Antibody Treatment Conquer Leukemia by Targeting Immune Suppression?
"A novel bispecific antibody shows promise in not only attacking leukemia cells but also dismantling the defenses they use to evade the immune system, potentially revolutionizing AML therapy."
Acute myeloid leukemia (AML) remains a formidable challenge in adult oncology, characterized by aggressive progression and a stubbornly low long-term survival rate of under 30%. Recent studies increasingly highlight the role of immune evasion in AML, suggesting that leukemia cells can cleverly dodge or suppress the body's natural defenses, leading to relapse and treatment failure. This has spurred interest in innovative immunotherapeutic approaches that can restore or enhance anti-leukemic immunity.
Among the key players in this immune evasion are myeloid-derived suppressor cells (MDSCs), a heterogeneous population of immune cells that share the ability to suppress T-cell responses. MDSCs accumulate in AML patients and create an environment that shields leukemia cells from immune attack, hindering the effectiveness of conventional therapies. Therefore, strategies to eliminate or neutralize MDSCs are gaining traction as a means to boost anti-leukemic immunity.
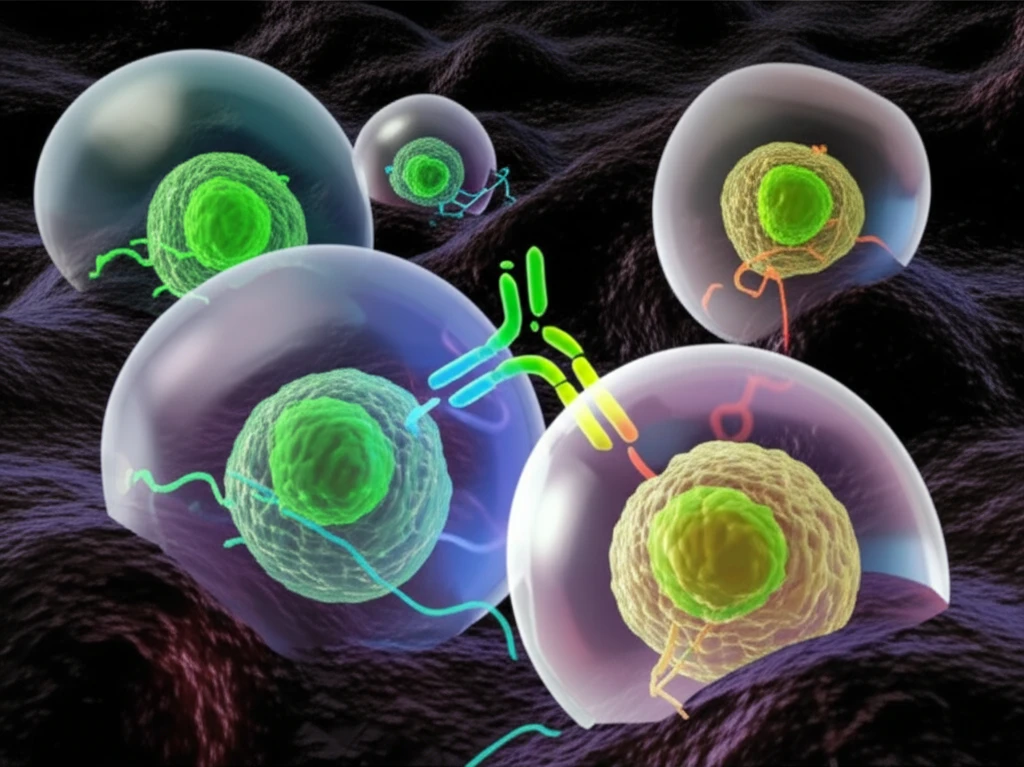
Now, researchers are exploring a promising approach using a bispecific antibody called AMG 330, which is designed to simultaneously target CD33, a protein expressed on both AML cells and MDSCs, and CD3, a protein on T cells. By bringing these cells together, AMG 330 aims to redirect T cells to eliminate both leukemia cells and immune-suppressing MDSCs, potentially offering a powerful two-pronged attack against AML.
Unveiling the Dual Action of AMG 330: A Novel Approach to AML Therapy
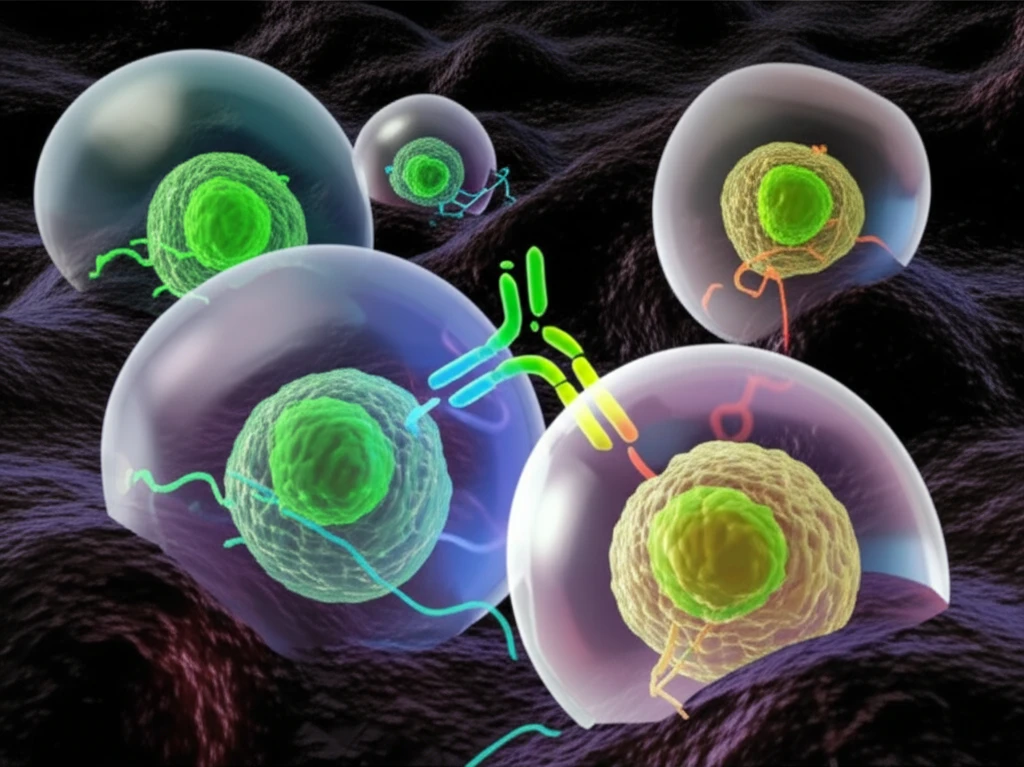
The groundbreaking research published in the Journal for ImmunoTherapy of Cancer sheds light on the potential of AMG 330 to overcome immune suppression in AML. The study reveals that AMG 330 not only targets and eliminates CD33-expressing AML cells but also effectively engages T cells to eradicate CD33+ MDSCs. This dual action is particularly significant because MDSCs are known to dampen the immune response and protect leukemia cells from destruction.
- Increased Frequencies of MDSCs in AML: The study confirms that patients with newly diagnosed AML have higher levels of CD14+ monocytic MDSCs that co-express CD33 but lack HLA-DR (HLA-DRlo).
- AML-Blasts Induce HLA-DRlo Cells: AML-blasts can induce HLA-DRlo cells from healthy donor-derived monocytes in vitro, which suppress T-cells and express indoleamine-2,3-dioxygenase (IDO).
- T-Cells Eliminate IDO+CD33+ MDSCs: T-cells eliminate IDO+CD33+ MDSCs in the presence of AMG 330.
- IDO Inhibition Promotes AML-Blast Clearance: IDO inhibition promotes AMG 330-mediated clearance of AML-blasts.
Future Directions: MDSCs as Predictors of Treatment Response
These findings suggest that AMG 330 may achieve anti-leukemic efficacy not only through T-cell-mediated cytotoxicity against AML-blasts but also against CD33+ MDSCs. The research team proposes exploring the predictive role of MDSCs for responsiveness towards an AMG 330-based therapy. By identifying patients with specific MDSC profiles, clinicians may be able to better tailor treatment strategies and improve outcomes in AML.
