AF & Heart Failure: Decoding the ICD Impact
"Is there a link between atrial fibrillation, heart failure, and implantable cardioverter-defibrillators?"
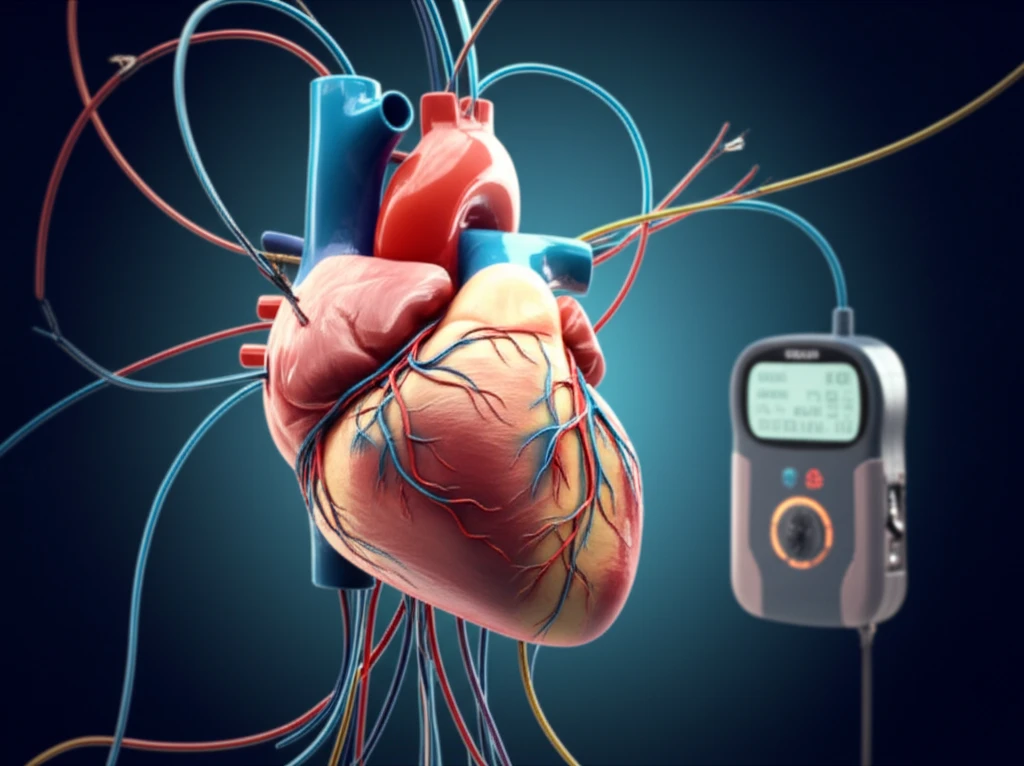
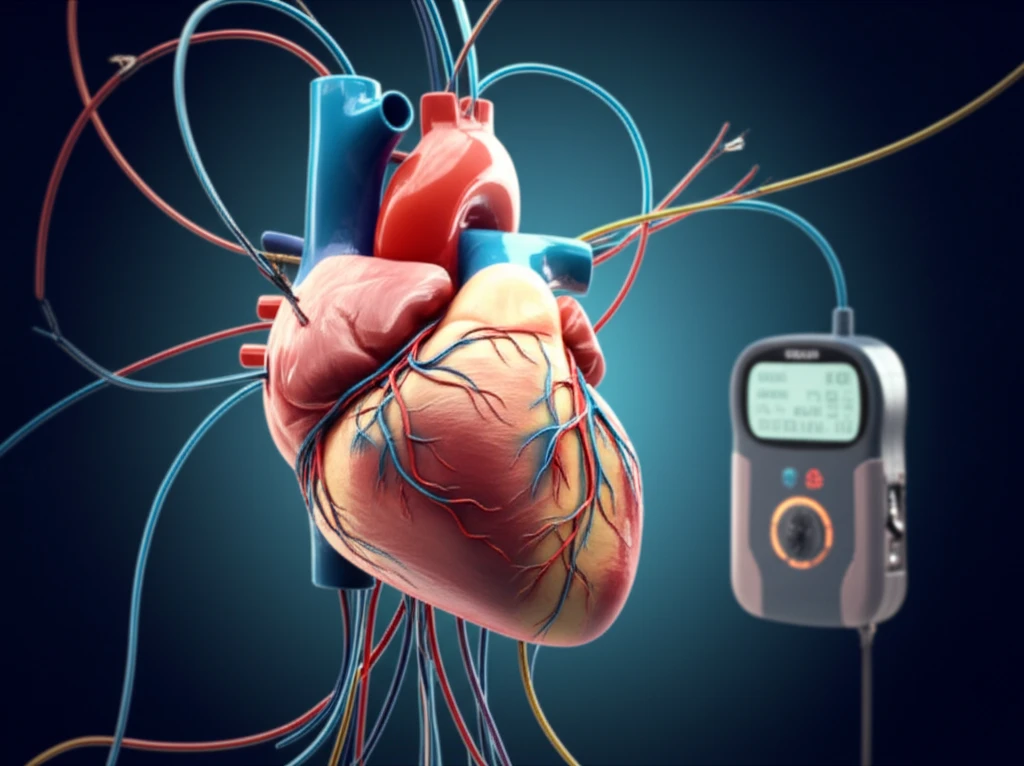
Atrial fibrillation (AF), a common heart rhythm disorder, is significantly more prevalent in individuals with heart failure (HF). While AF is known to increase the risk of HF, the relationship becomes even more complex when patients have an implantable cardioverter-defibrillator (ICD). ICDs are designed to prevent sudden cardiac death in at-risk individuals. But the interplay between AF, HF, and ICD therapies remains a subject of considerable debate and research.
The core of the issue lies in understanding whether AF independently worsens outcomes for HF patients with ICDs, or if it simply marks more advanced heart disease. Studies have presented conflicting results, leading to uncertainty about the true impact of AF in this specific patient population. Adding to the complexity, ICD therapies themselves, both appropriate and inappropriate, are associated with poorer prognoses.
To shed light on this complex relationship, a systematic review and meta-analysis was conducted, pooling data from multiple studies. This analysis sought to provide a clearer picture of how a history of AF impacts mortality and the occurrence of ICD therapies in patients with heart failure and reduced ejection fraction (HFrEF) who have an ICD.
Decoding the Link: AF, Heart Failure, and ICD Outcomes
Researchers conducted a thorough search of medical literature through November 2016, identifying 62 studies involving 227,998 patients. These studies explored the connection between AF and various outcomes in HF patients with ICDs. The analysis focused on three key areas: all-cause mortality, appropriate ICD therapies (shocks or anti-tachycardia pacing), and inappropriate ICD therapies.
- Increased Mortality: HF patients with a history of AF had a 42% higher risk of all-cause mortality.
- Appropriate ICD Therapies: AF patients faced a higher risk of receiving appropriate ICD therapies.
- Inappropriate ICD Therapies: These patients also had a significantly elevated risk of inappropriate ICD interventions.
The Big Picture: Implications and Future Directions
This comprehensive review reinforces the importance of atrial fibrillation as a critical factor in managing heart failure patients with ICDs. The increased risks of mortality and ICD interventions highlight the need for proactive strategies to address AF in this population.
While the study clarifies the association, it also raises important questions about the nature of the relationship. Is AF simply a marker of more severe heart failure, or does it actively contribute to poorer outcomes? Further research is needed to dissect the independent impact of AF.
Moving forward, better characterization and detailed phenotyping of HF patients with ICDs are essential. This would allow for the identification of HF patients who would benefit from surveillance of AF prevention and also aggressive rhythm control.
