Acetazolamide and Skin Reactions: What You Need to Know
"A rare case highlights a potential link between acetazolamide, a common medication, and unique skin eruptions. Learn about symptoms, diagnosis, and implications."
Allergic and adverse reactions to sulfonamide medications are relatively common. While acetazolamide, a type of sulfonamide, is generally well-tolerated, it can occasionally lead to cutaneous adverse drug reactions (CADRs). These reactions can manifest in various ways, including maculopapular exanthemas, acute generalized exanthematous pustulosis (AGEP), and Stevens-Johnson syndrome.
This article reports a unique case of a lichenoid and pigmented drug eruption triggered by oral acetazolamide, confirmed through a lichenoid patch test. This is the first documented case of its kind, offering valuable insights into the potential dermatological side effects of this medication.
The case involves a 76-year-old patient who developed a pruriginous maculopapular rash after being prescribed oral acetazolamide to prevent vitreous loss during cataract surgery. The rash initially appeared in the large folds of the skin, specifically in the submammary, inguinal, and axillary areas, without any mucosal involvement.
Unusual Symptoms and Diagnosis
The patient's condition evolved rapidly. Although pustules weren't initially observed, the skin lesions progressed to a fine desquamation, a characteristic sign observed during the healing phase of AGEP. Clinical examination revealed the patient was afebrile but presented with bilateral axillary lymphadenopathy and mild facial edema.
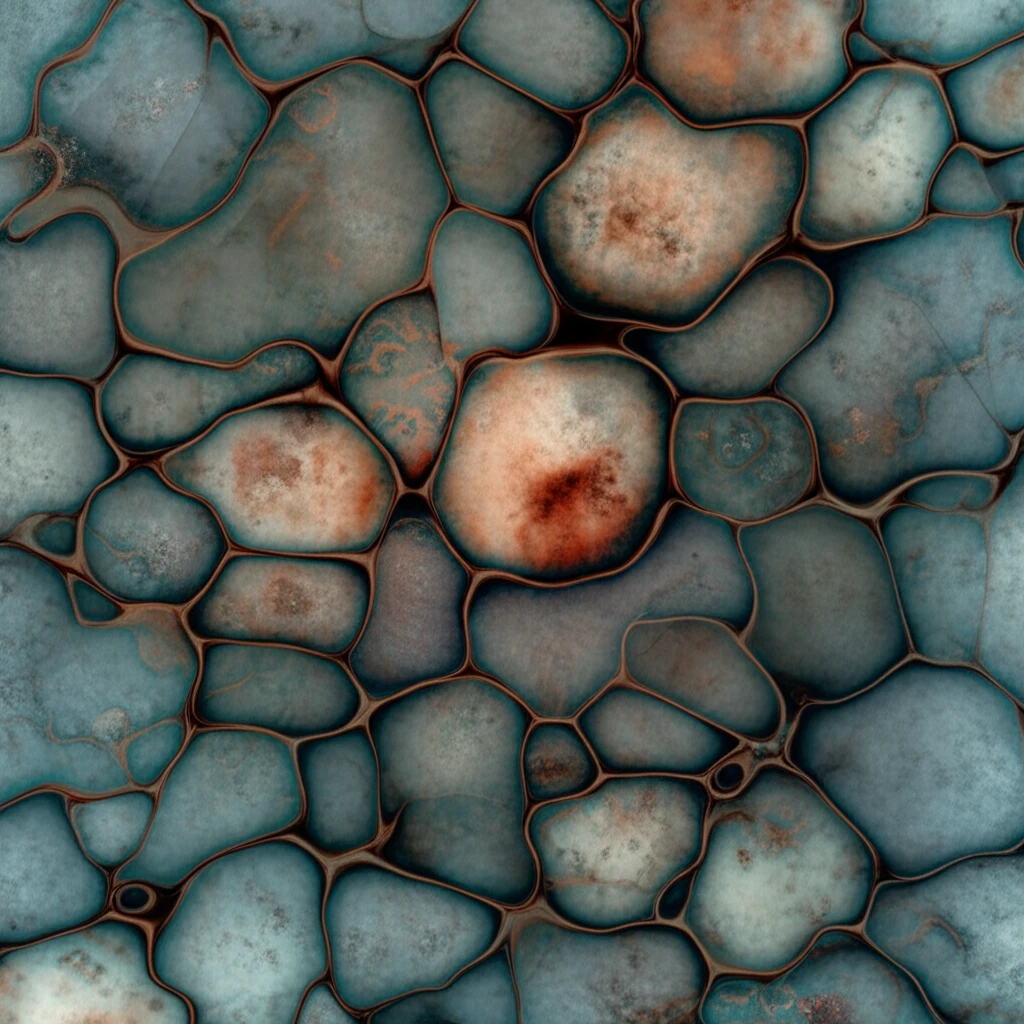
- Lichenoid Pattern: Characterized by a band-like infiltrate of lymphocytes in the upper dermis.
- Hyperpigmentation: Development of hyperpigmented skin patches in previously affected areas.
- Patch Test Confirmation: Positive patch tests for acetazolamide confirmed the diagnosis.
Implications and Further Considerations
This case underscores the importance of considering acetazolamide as a potential cause of lichenoid and pigmented drug eruptions, even though such reactions are rare. The positive patch test results emphasize the value of patch testing in assessing drug imputability and confirming the diagnosis.
While the initial presentation resembled AGEP, the progression to hyperpigmented skin and the lichenoid pattern observed in biopsies differentiated it from typical AGEP cases. This highlights the importance of careful clinical and histopathological evaluation in diagnosing unusual drug reactions.
This case expands the spectrum of known cutaneous side effects associated with acetazolamide and emphasizes the need for clinicians to be aware of these potential reactions. Further research is needed to understand the underlying mechanisms and risk factors associated with acetazolamide-induced lichenoid and pigmented drug eruptions.
