Unlocking Precision: How Dual-Balloon Catheters are Revolutionizing Liver Cancer Treatment
"Discover how a novel dual-balloon catheter technique is enhancing targeted drug delivery in liver cancer therapy, minimizing side effects and improving patient outcomes."
Liver cancer, particularly hepatocellular carcinoma (HCC), poses a significant challenge in oncology due to its complex vascular structure and tendency to develop resistance to conventional treatments. Transarterial chemoembolization (TACE) has long been a cornerstone of HCC management, but its effectiveness can be limited by incomplete tumor embolization and the potential for non-target effects. This is where innovative techniques come into play, aiming to refine the precision and efficacy of intra-arterial therapies.
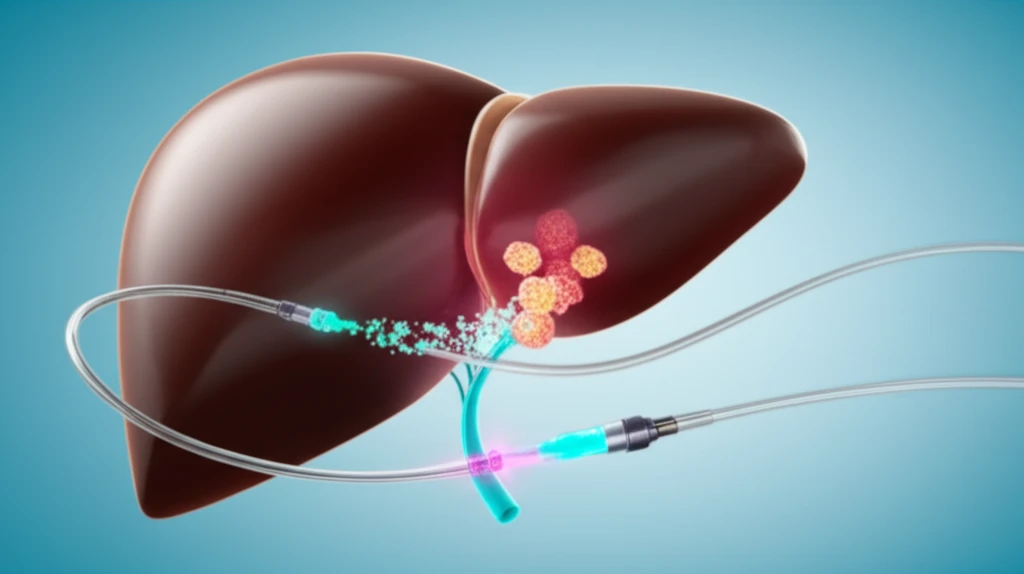
One such innovation is the use of dual-balloon catheters, which offer a unique approach to isolating and treating target vessels within the liver. By creating a controlled environment, these catheters enable more focused drug delivery, reducing the risk of exposing healthy tissue to toxic agents. This method is particularly valuable in cases where traditional superselective positioning is difficult or when treating hypovascular tumors that require enhanced agent penetration.
This article delves into the mechanics, benefits, and potential limitations of dual-balloon catheter techniques in liver cancer therapy. We'll explore how this approach is transforming the landscape of interventional radiology, offering new hope for patients with complex HCC cases and pushing the boundaries of what's possible in targeted cancer treatment.
Targeted Therapy: How Dual-Balloon Catheters Enhance Drug Delivery
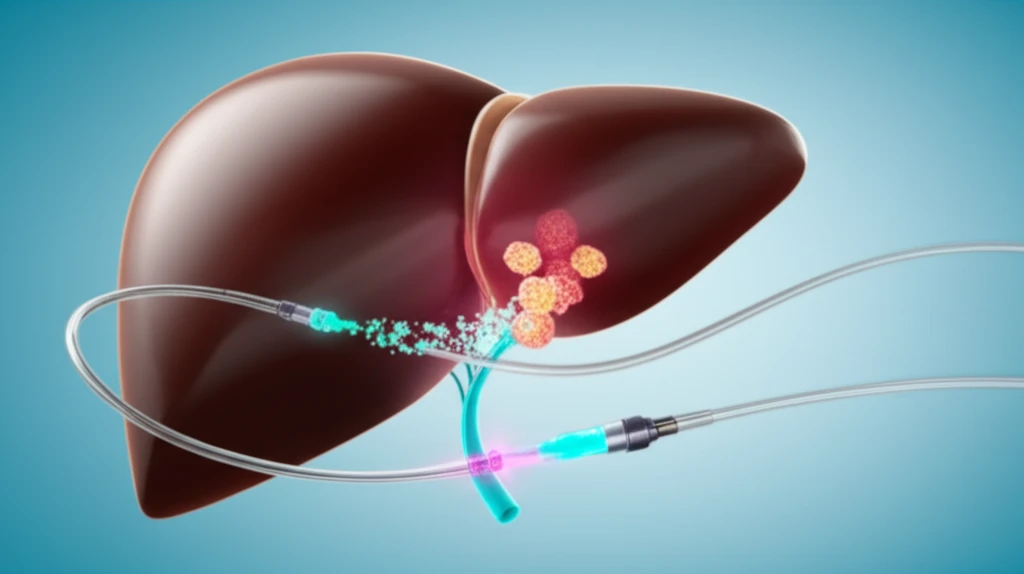
Dual-balloon catheters represent a significant advancement in targeted cancer therapy, particularly for liver tumors. Unlike traditional methods that rely on a single point of access, these catheters use two inflatable balloons to create a temporary, isolated segment within the blood vessels supplying the tumor. This isolation allows for the direct infusion of therapeutic agents, such as chemotherapy drugs or embolic materials, into the tumor site while minimizing the risk of reflux or leakage into surrounding healthy tissues.
- Precise drug delivery: Minimizes exposure of healthy tissue to toxic agents.
- Customizable isolation: Adjustable balloon-to-balloon length to match target vessel size.
- Controlled infusion: Variable balloon pressures for optimal drug penetration.
- Reduced non-target embolization: Decreases the risk of reflux or leakage.
- Simultaneous treatment: Ability to target multiple tumor branches.
The Future of Liver Cancer Therapy: A Call for Further Research
While dual-balloon catheter techniques show great promise in enhancing the precision and effectiveness of liver cancer treatment, it's important to acknowledge the limitations and areas for future research. The current generation of catheters can be expensive compared to standard microcatheters, and their use requires specialized training and expertise. Additionally, more studies are needed to fully understand the hemodynamic effects of balloon occlusion and how they impact therapeutic agent delivery. By addressing these challenges, we can further refine this innovative approach and unlock its full potential to improve outcomes for patients with liver cancer.
