Takayasu Arteritis and Your Eyes: What You Need to Know
"Understanding the ocular manifestations of Takayasu arteritis and how early detection can protect your vision."
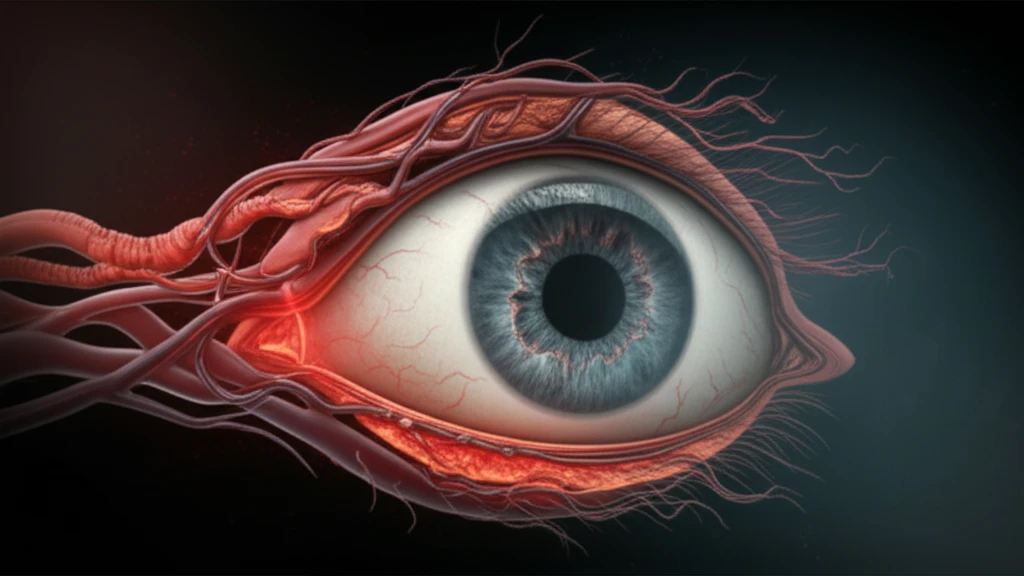
Takayasu arteritis is a rare, chronic inflammatory disease affecting the aorta and its major branches. While it's known for its impact on major arteries, many people don't realize it can also affect the eyes. Because the condition reduces blood flow, it can cause a range of eye-related issues, some of which can lead to vision loss if not addressed promptly.
This condition, sometimes called "pulseless disease" because it can weaken or eliminate pulses in the arms or legs, primarily affects young women, typically between the ages of 20 and 40. Recognizing the potential ocular manifestations of Takayasu arteritis is crucial for early diagnosis and management, helping to preserve vision and overall quality of life.
This article breaks down the connection between Takayasu arteritis and eye health, explaining the specific ways this arteritis can manifest in your eyes. We'll also cover the importance of early detection, available treatment options, and what steps you can take to protect your vision if you have been diagnosed with Takayasu arteritis.
How Does Takayasu Arteritis Affect the Eyes?
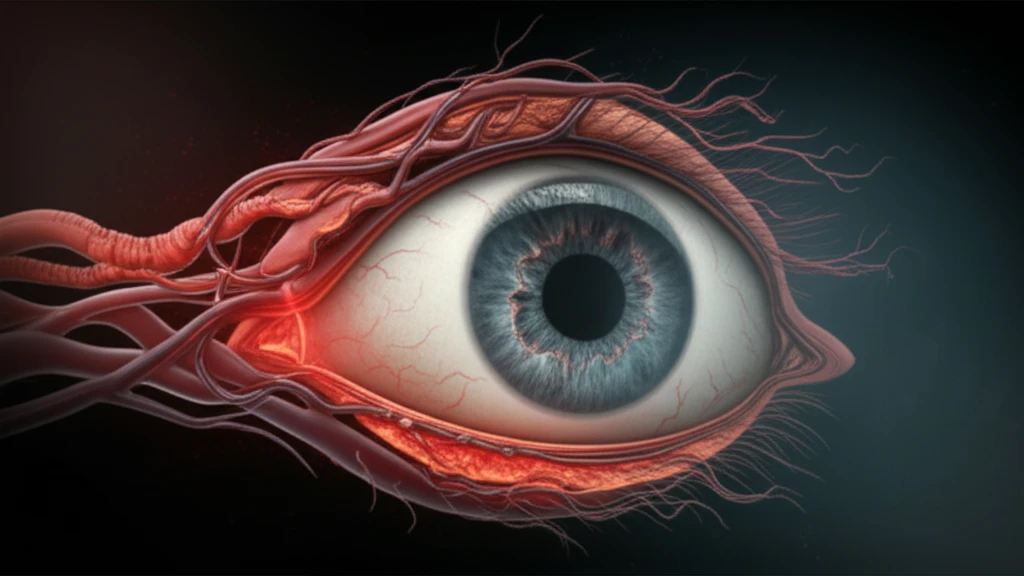
Takayasu arteritis can impact the eyes in two primary ways: through hypoperfusion (reduced blood flow) and hypertension (high blood pressure). The specific manifestations depend on which arteries are affected and the severity of the inflammation. Here are some potential ocular issues associated with Takayasu arteritis:
- Ocular Ischemic Syndrome (OIS): Reduced blood flow to the eye can lead to OIS, characterized by symptoms like eye pain, vision loss, and light sensitivity. Examination may reveal signs of retinal ischemia, such as arteriolar narrowing, microaneurysms, and neovascularization (the growth of new, abnormal blood vessels).
- Anterior Ischemic Optic Neuropathy (AION): Inflammation and reduced blood flow can damage the optic nerve, leading to AION. This condition causes sudden vision loss, often painless, and can result in permanent visual impairment.
- Takayasu Retinopathy: This specific retinopathy is characterized by changes in the retinal blood vessels, including venous dilation, microaneurysms, and arteriovenous anastomoses (abnormal connections between arteries and veins). In advanced stages, it can lead to retinal ischemia, neovascularization, and vitreous hemorrhage.
- Central Retinal Artery Occlusion: Although rare, Takayasu arteritis can cause a blockage in the central retinal artery, leading to sudden and severe vision loss.
Protecting Your Vision
If you have Takayasu arteritis, regular eye exams are essential. Early detection and management of ocular manifestations can significantly reduce the risk of vision loss. Work closely with your rheumatologist and ophthalmologist to develop a comprehensive treatment plan that addresses both the systemic inflammation and any eye-related issues.
