Stent Pain Relief: Does Lidocaine Hold the Key?
"A randomized study explores the effectiveness of intraureteral lidocaine for managing post-ureteroscopy stent symptoms, offering insights into alternative pain relief strategies."
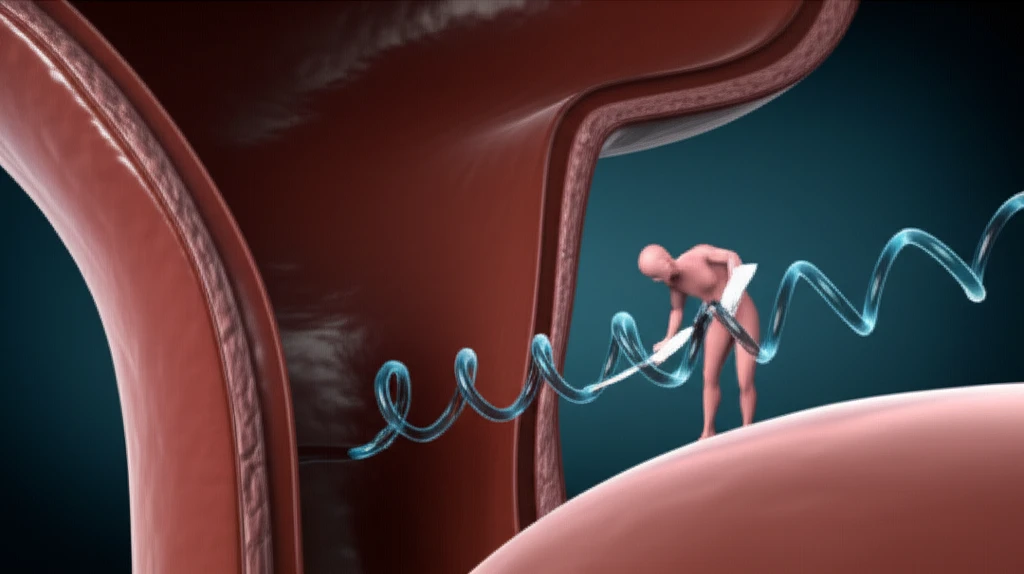
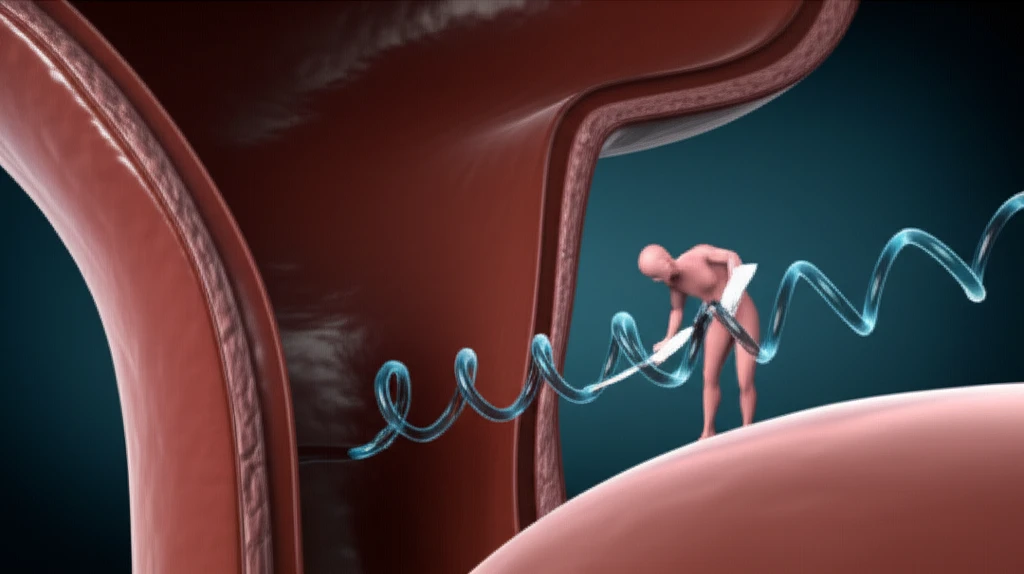
Ureteroscopy (URS) has become a cornerstone treatment for kidney and ureteral stones. Often, a small tube called a ureteral stent is placed after the procedure to aid healing. However, many patients experience pain and discomfort related to these stents, impacting their quality of life.
Traditional approaches to manage stent-related symptoms include oral medications, modified stent designs, and even drug-eluting stents. Yet, the problem persists, prompting researchers to explore novel solutions. One such approach involves delivering medication directly into the urinary tract.
A study published in the Canadian Urological Association Journal investigated the use of intraureteral lidocaine—a local anesthetic—to alleviate pain and urinary symptoms after ureteroscopy. This randomized, placebo-controlled trial aimed to determine if direct instillation of lidocaine could provide significant relief.
The Lidocaine Study: A Deep Dive into Design and Results
The study enrolled 41 patients undergoing elective ureteroscopy for kidney or ureteral stones. Following stone removal, participants were randomly assigned to receive either intraureteral lidocaine plus bicarbonate or a normal saline solution. Pain levels were assessed using a visual analog scale (VAS) at various time points, including one hour, two hours, four hours, 24 hours, four days, and seven days after the procedure. Researchers also collected data on medication use and urinary symptoms.
- No Significant Pain Reduction: The study found no statistically significant difference in pain scores between the lidocaine and placebo groups at any time point.
- Modest Improvement in Dysuria: Patients in the lidocaine group reported slightly lower dysuria scores, but the difference did not reach statistical significance.
- Similar Complication Rates: The incidence of complications and adverse effects was comparable between the two groups.
Future Directions: Finding Better Solutions for Stent Discomfort
Although intraureteral lidocaine may not be the definitive answer, this study contributes valuable insights to the ongoing quest for effective stent pain management. Further research is needed to explore alternative approaches, such as different anesthetic agents, optimized delivery techniques, or combination therapies. In the meantime, open communication with your urologist is key to finding the best strategy to manage stent-related symptoms and improve your overall well-being.
