Sleep After Brain Injury: Why It Matters and How to Navigate Challenges
"Understanding the Link Between Sleep Disturbances and Recovery, Plus Practical Tips for Better Rest."
Traumatic brain injury (TBI) can be a life-altering event, and the journey to recovery is often complex. While the physical and cognitive challenges are well-known, the impact of sleep disturbances is frequently overlooked. However, emerging research highlights a significant link between sleep quality and the overall recovery process after TBI. This article delves into the critical connection between sleep and neurobehavioral impairments, providing insights and actionable strategies for better sleep.
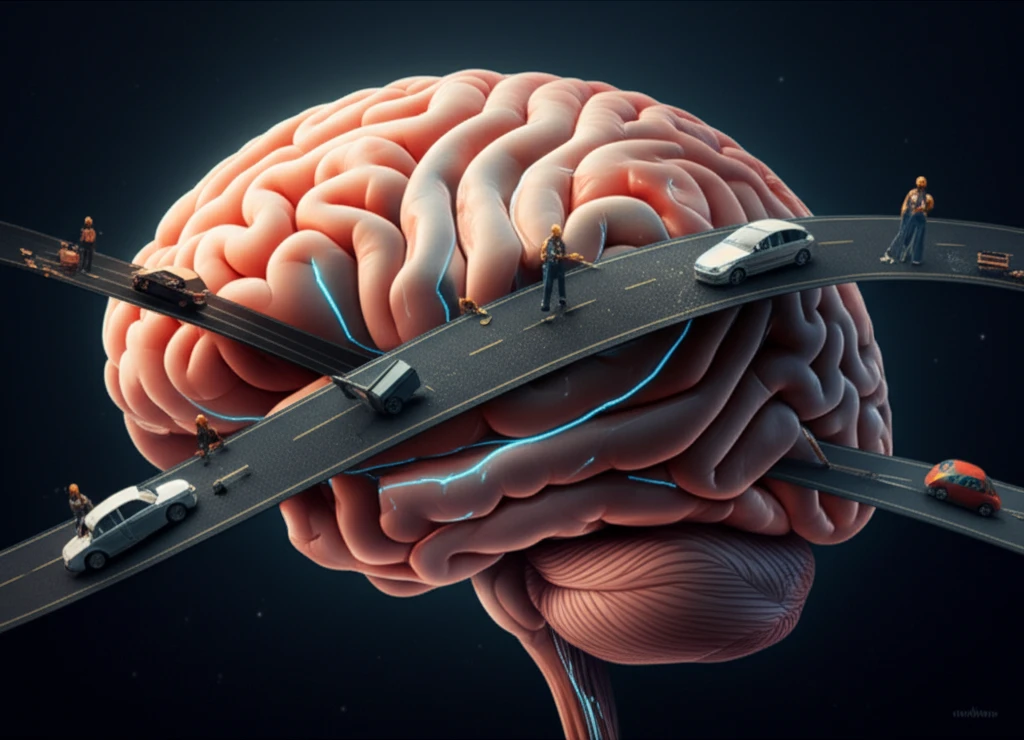
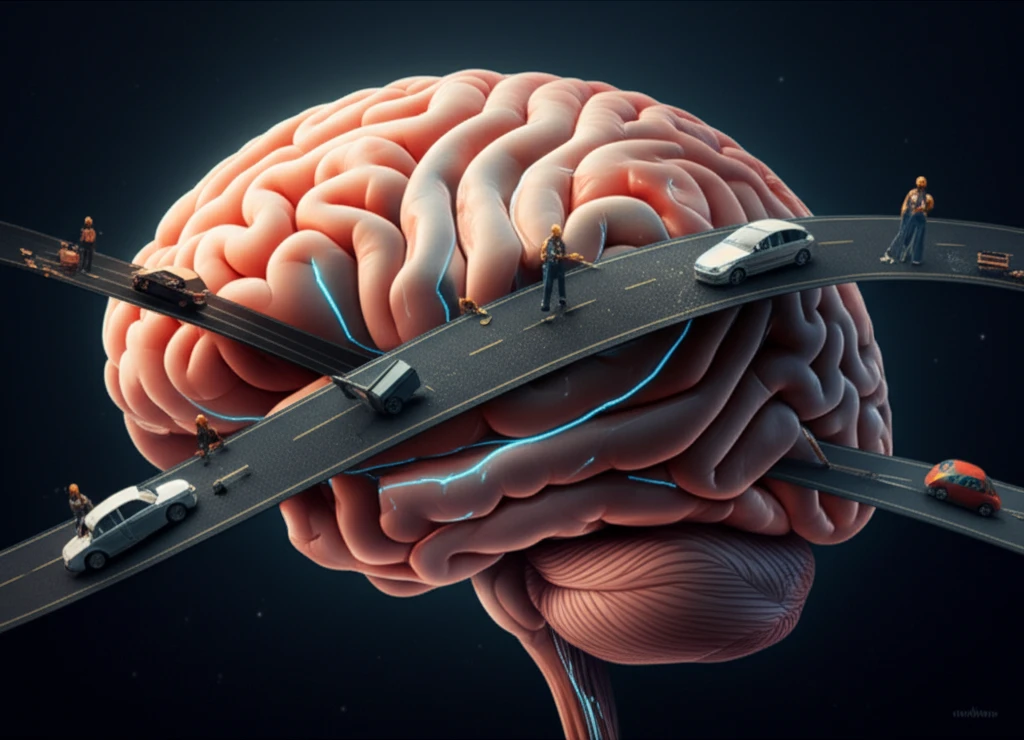
Imagine your brain as a busy city. After a TBI, the roads (neural pathways) might be damaged, leading to traffic jams (cognitive impairments). Sleep is like a nightly repair crew, working to fix the roads and restore order. When sleep is disrupted, the repair work suffers, exacerbating existing problems and hindering recovery. This is why understanding and addressing sleep issues is so crucial after TBI.
This article aims to shed light on the relationship between sleep and neurobehavioral impairments, offering practical advice and guidance. We'll explore why sleep matters, how it impacts recovery, and what steps individuals, caregivers, and healthcare providers can take to improve sleep quality and enhance overall well-being. Whether you're a TBI survivor, a caregiver, or a healthcare professional, this information can make a difference.
The Unseen Enemy: How Sleep Disruptions Affect Recovery After TBI
Sleep disturbance is a common issue following a TBI, with studies showing that a significant percentage of individuals experience sleep disorders like insomnia and hypersomnia. These sleep problems aren't just about feeling tired; they can profoundly affect various aspects of recovery. Research consistently demonstrates a strong correlation between sleep disturbances and neurobehavioral impairments.
- Cognitive Deficits: Difficulty with attention, memory, and executive functions.
- Mood Disorders: Increased risk of depression, anxiety, and emotional dysregulation.
- Behavioral Changes: Irritability, impulsivity, and social difficulties.
- Reduced Participation: Impaired ability to engage in rehabilitation therapies.
Taking Action: Practical Steps for Better Sleep and Recovery
Addressing sleep disturbances is a critical component of the TBI recovery process. By understanding the link between sleep and neurobehavioral impairments, individuals, caregivers, and healthcare providers can work together to improve sleep quality and enhance overall well-being. Prioritizing sleep is not just about getting a good night's rest; it's about supporting the brain's natural healing processes and optimizing the chances for a successful recovery. Remember, every step taken towards better sleep is a step towards a brighter future after TBI.
