Sickle Cell Retinopathy: Clearing Up the Confusion
"Navigating the Terminology and Diagnosis for Better Outcomes"
A recent study by Beral and associates shed light on the prevalence of retinopathy and maculopathy in patients with sickle cell disease (SCD), noting the absence of a direct link to hematological parameters, blood rheology, or genotype. While this research contributes valuable insights, it also highlights the need for clear and consistent terminology in the diagnosis and classification of these conditions.
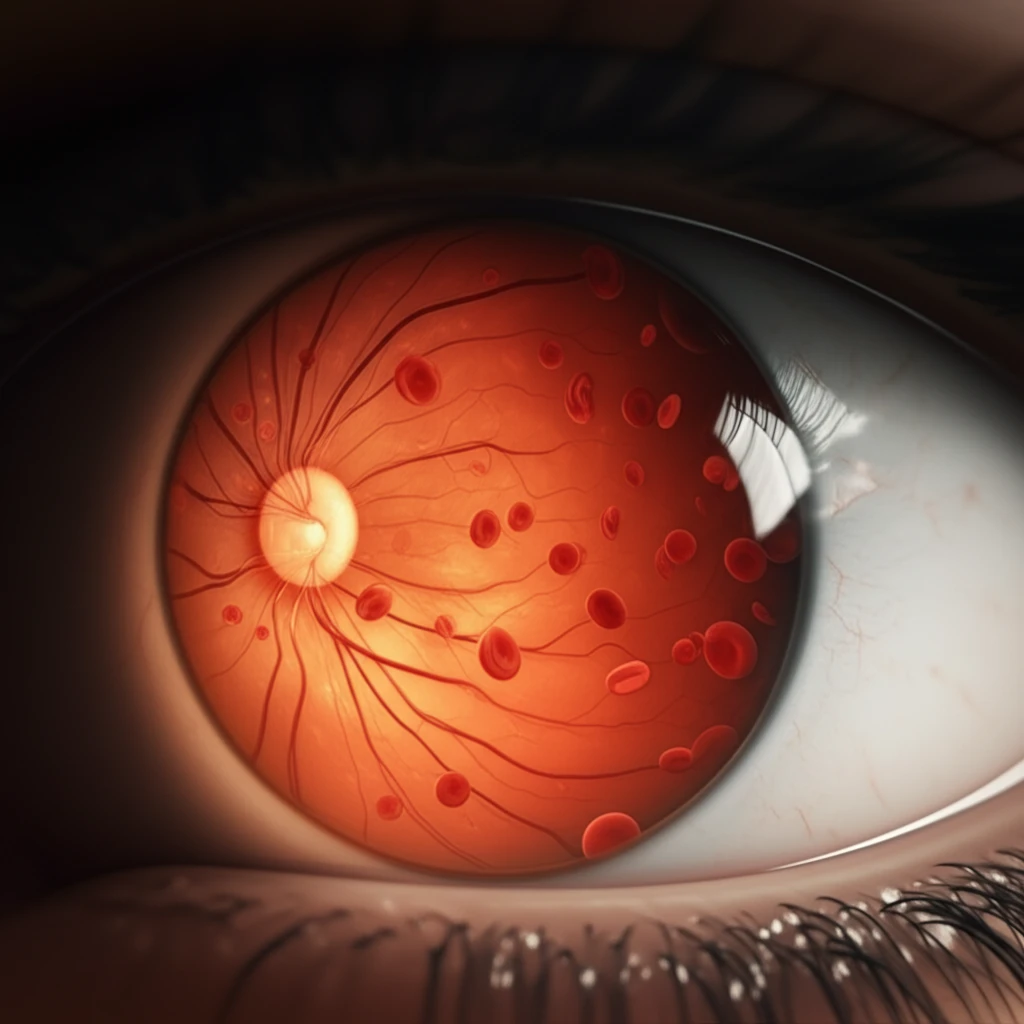
The retina, a complex structure essential for vision, is divided into the posterior pole and the peripheral retina. Within the posterior pole lies the macula, a critical area for central vision. General terms like 'retinopathy' and 'maculopathy' simply refer to diseases affecting the retina and macula, respectively. However, when dealing with specific conditions like sickle cell retinopathy (SCR), a more detailed approach is crucial.
Since Goldberg's classification of SCR in 1971, it has served as the gold standard for diagnosing and classifying the disease through funduscopic examination. Macular involvement in SCD was first described in 1972, with traction maculopathy already recognized as related to proliferative SCR. Maculopathy is, therefore, an integral component of SCR, closely linked to peripheral vascular nonperfusion.
Retinopathy vs. Maculopathy: Defining the Terms in Sickle Cell Disease
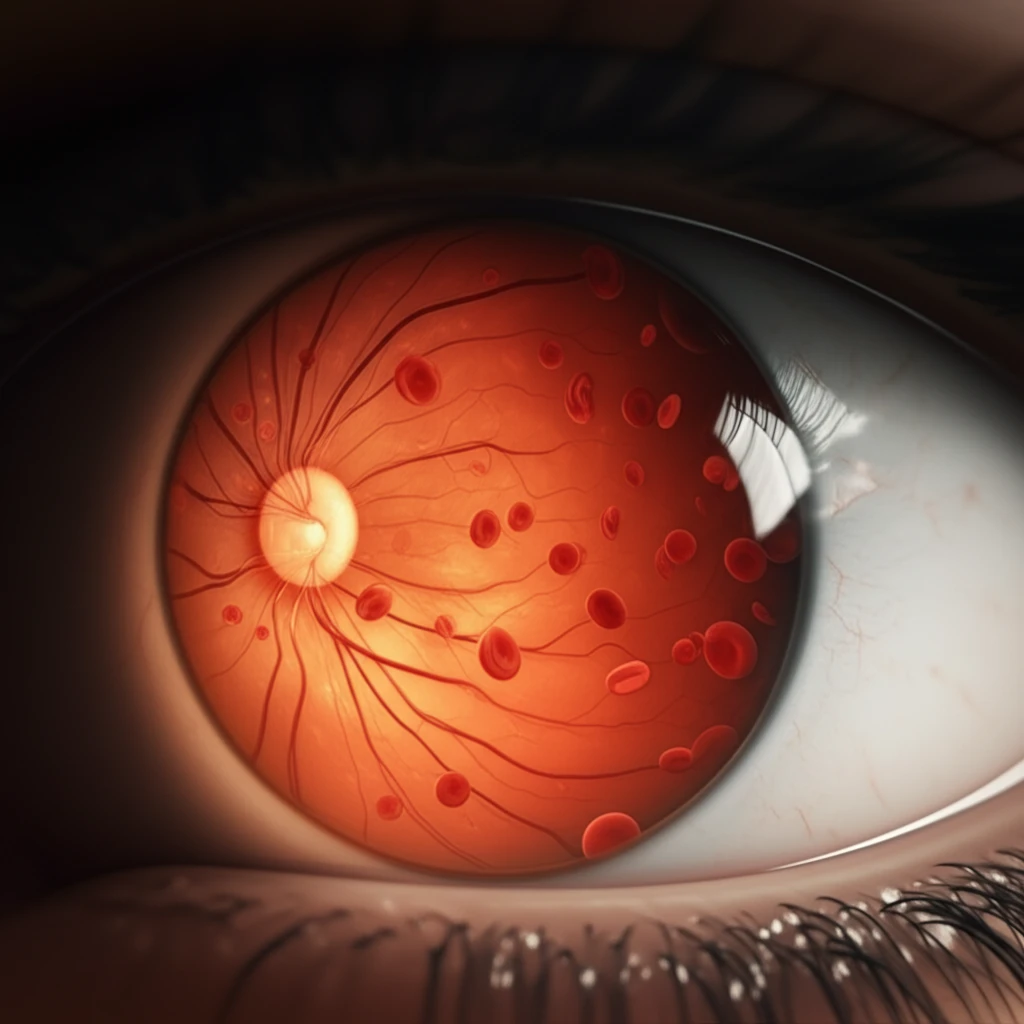
The study by Beral and colleagues employs the terms 'Retinopathy' and 'Maculopathy' seemingly as distinct entities. However, the diagnostic criteria and classifications used for each were not clearly defined. This raises questions about how 'Retinopathy' (peripheral vascular alterations) and 'Maculopathy' (macular ischemic impairment) were specifically assessed, and what stage of peripheral retinopathy and OCT findings were considered for diagnosis.
- Fluorescein Angiography (FA): Detects peripheral SCR stages earlier.
- Optical Coherence Tomography (OCT): More sensitive for detecting sickle cell maculopathy.
Moving Forward: Toward Enhanced Diagnostic Protocols
Clarifying the diagnostic criteria for retinopathy and maculopathy is crucial. Distinguishing between peripheral vascular changes and macular involvement is essential for accurate diagnosis and treatment planning.
The Dell'Arti et al. study highlights the potential of OCT technology in identifying systemic risk factors associated with sickle cell maculopathy, and suggests that chronic chelation therapy and elevated HbF levels may offer protective benefits. This underscores the importance of continued research into both diagnostic and therapeutic strategies.
By refining diagnostic approaches and incorporating advanced imaging techniques, healthcare professionals can improve early detection and management of SCR and maculopathy, ultimately preserving vision and enhancing the quality of life for individuals with sickle cell disease.
