Liver Cancer Treatment: Is Retrograde Portal Vein Flow a Red Flag?
"Decoding the Impact of Portal Vein Flow on TACE Outcomes in Hepatocellular Carcinoma Patients"
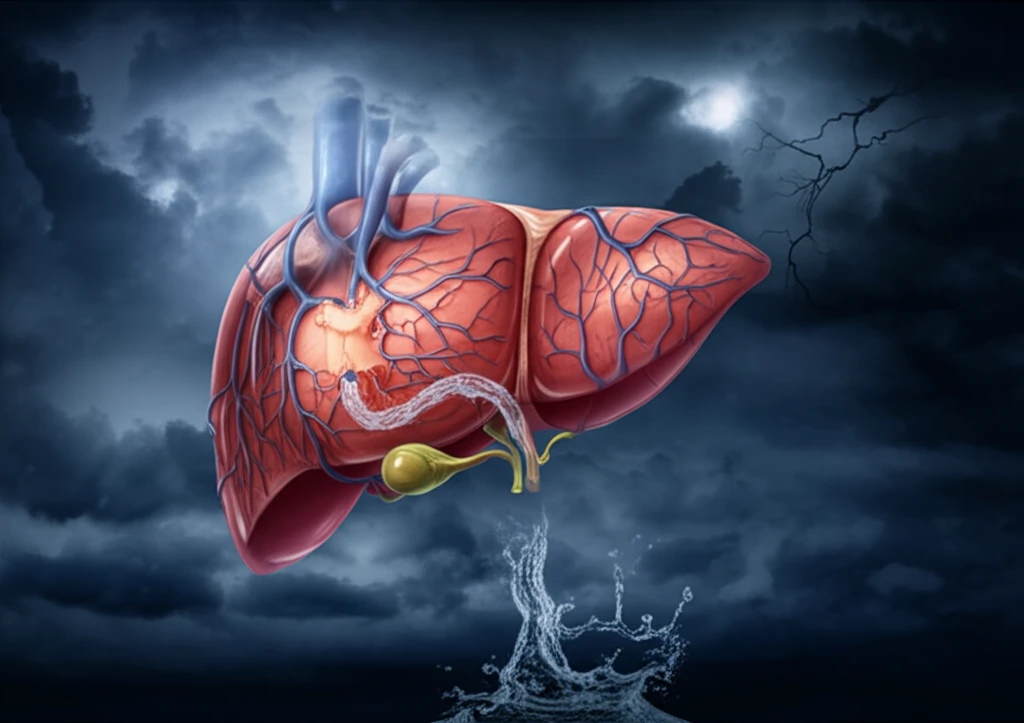
Hepatocellular carcinoma (HCC), the most common type of liver cancer, poses a significant global health challenge. Often diagnosed at advanced stages, HCC requires complex treatment strategies. Transarterial chemoembolization (TACE) has emerged as a primary treatment for intermediate-stage HCC, offering a lifeline to many. But what happens when the liver's natural blood flow is disrupted?
The liver receives blood from two major vessels: the hepatic artery and the portal vein. The portal vein is responsible for around 75% of the liver's blood supply, carrying nutrient-rich blood from the digestive system. When this flow is reversed, known as retrograde portal vein flow, it can signal severe portal hypertension and advanced liver disease. This reversal can complicate HCC treatment, potentially impacting the effectiveness of TACE.
A new study published in the Scandinavian Journal of Gastroenterology investigates whether retrograde portal vein flow affects the outcomes of TACE in HCC patients. The study aims to determine if TACE in patients with reversed portal vein flow leads to a greater decline in liver function and poorer survival rates compared to those with normal (orthograde) flow. By understanding these dynamics, medical professionals can better tailor treatment approaches, especially in borderline cases.
Unpacking the Study: TACE and Portal Vein Flow
Researchers at Hannover Medical School in Germany conducted a retrospective analysis of 407 HCC patients treated with TACE. These patients had undergone Doppler ultrasound to assess portal vein flow before treatment. The study divided participants into two groups: those with normal (orthograde) portal vein flow and those with reversed (retrograde) flow. The goal was to compare overall survival (OS) and changes in liver function between the groups.
- Significantly more often liver cirrhosis.
- Advanced hepatic dysfunction.
- Retrograde PV flow group had a median survival of 12 months vs 19 in the orthograde group.
Clinical Implications and Future Directions
The study highlights the importance of assessing portal vein flow before TACE treatment in HCC patients, especially for those with advanced liver disease. While retrograde portal vein flow alone does not contraindicate TACE, it serves as a signal for caution and may warrant a more individualized treatment plan. Further research, including larger prospective studies, could refine our understanding of the interplay between portal hemodynamics and TACE outcomes. By identifying patients at higher risk, clinicians can explore alternative or adjunctive therapies to improve survival and quality of life. This personalized approach promises to optimize outcomes and enhance the care for those battling this challenging cancer.
