Leptin's Unexpected Role: How It Impacts Neuropathic Pain After Spinal Cord Injuries
"Discover the surprising connection between leptin, inflammation, and nerve pain following preganglionic cervical root avulsion."
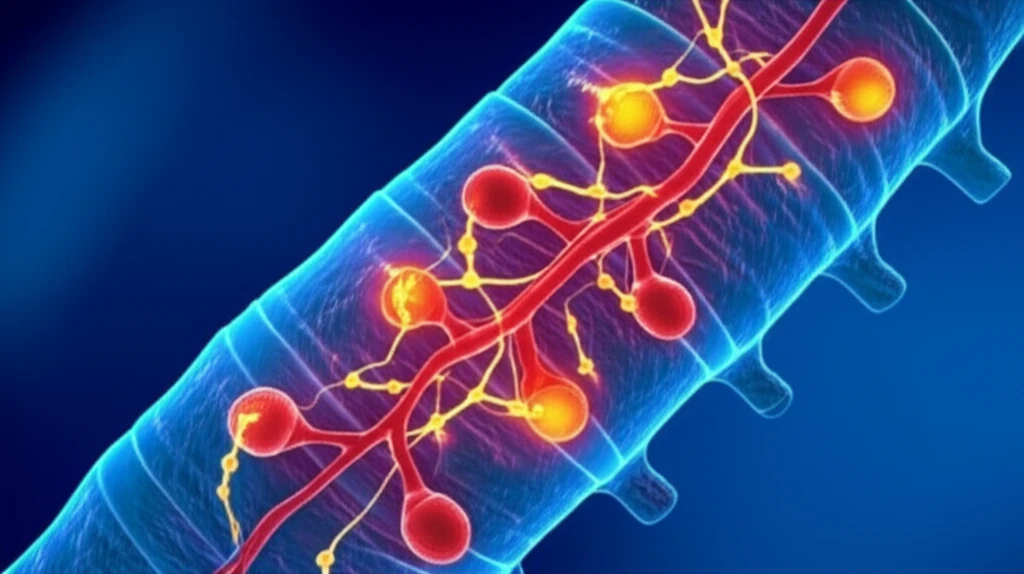
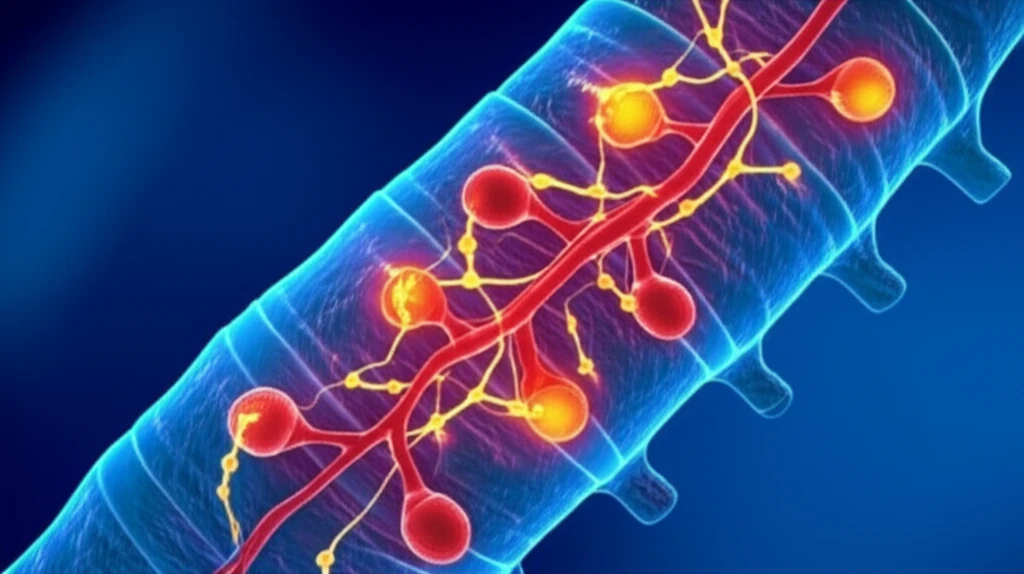
Spinal cord injuries, particularly preganglionic cervical root avulsion (PCRA), can lead to a cascade of debilitating effects, including chronic neuropathic pain. This type of pain arises from damage to the nervous system itself, often proving resistant to conventional treatments. Unlike typical nerve injuries, PCRA involves the disruption of nerve roots at the spinal cord, creating unique challenges for pain management.
Researchers have long sought to understand the mechanisms that drive neuropathic pain following spinal cord injuries. One key area of investigation centers on the role of inflammation and immune responses within the nervous system. Microglia, the resident immune cells of the brain and spinal cord, become activated after injury and contribute to the inflammatory environment that can sensitize nerves and amplify pain signals.
Now, a recent study has shed light on the surprising involvement of leptin, a hormone primarily known for its role in regulating appetite and metabolism, in the development of neuropathic pain after PCRA. This research reveals that leptin plays a critical role in activating microglia and promoting inflammation within the spinal cord, ultimately contributing to the persistence of nerve pain.
Leptin: More Than Just an Appetite Regulator
Leptin, produced by fat cells, signals to the brain to regulate hunger and energy expenditure. However, its functions extend far beyond appetite control. Leptin is also involved in immune responses and inflammation. This dual role makes it a fascinating subject for researchers investigating the complex interplay between metabolism, immunity, and pain.
- Microglial Activation: Leptin directly stimulated microglia, causing them to become more active and release inflammatory substances.
- Increased Inflammatory Markers: Leptin increased the expression of CD86 and iNOS, key markers of microglial activation and inflammation.
- Demyelination: Leptin promoted the breakdown of myelin, the protective sheath around nerve fibers, further contributing to nerve damage and pain.
- Allodynia: Mice with higher leptin activity exhibited allodynia, a condition where normally harmless stimuli, such as a light touch, become painful.
Future Directions: Targeting Leptin for Pain Relief
This research opens exciting new avenues for treating neuropathic pain following spinal cord injuries. By targeting leptin and its inflammatory effects, researchers hope to develop more effective pain management strategies. Future studies will focus on identifying specific inhibitors of leptin signaling pathways and exploring their potential to alleviate chronic nerve pain. Understanding leptin's role is crucial for developing targeted therapies that can improve the quality of life for individuals suffering from spinal cord injuries.
