Heart Failure SOS: Spot the Signs & Slash Your Risk
"Decoding acute heart failure and pulmonary edema for women under 40."
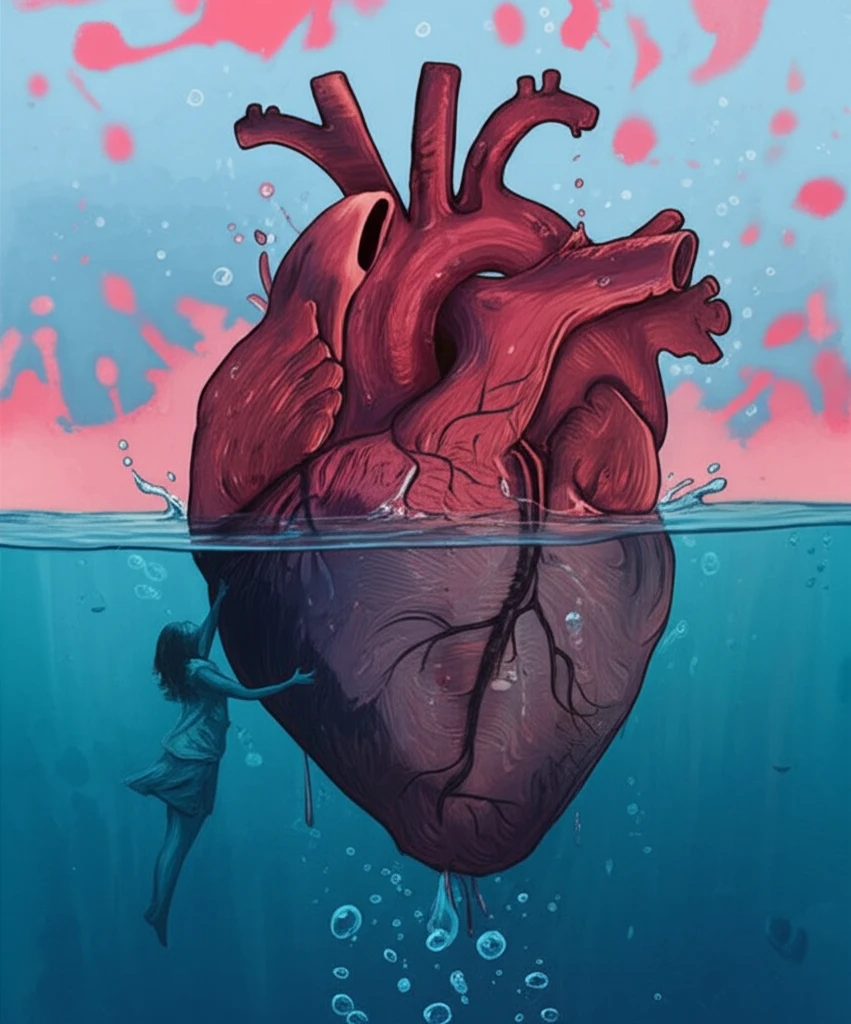
Imagine feeling like you're drowning – gasping for air, your chest tight, and panic rising. That's the terrifying reality of acute heart failure (AHF), a sudden and severe condition where your heart can't pump enough blood to meet your body's needs. It often leads to urgent hospital visits, and for many, it's a recurring nightmare.
But what exactly is AHF, and why is it so critical to understand, especially for women? It's more than just a 'heart problem'. AHF is a complex syndrome with various triggers and faces. Recognizing the signs early can be life-saving. We're breaking down the science, ditching the jargon, and giving you the actionable steps you need to protect your heart.
While often associated with older adults, AHF can strike at any age. Understanding the risk factors, symptoms, and treatment options is essential for proactive health management. Let's get informed and empowered.
Unpacking Acute Heart Failure: What's Really Happening?
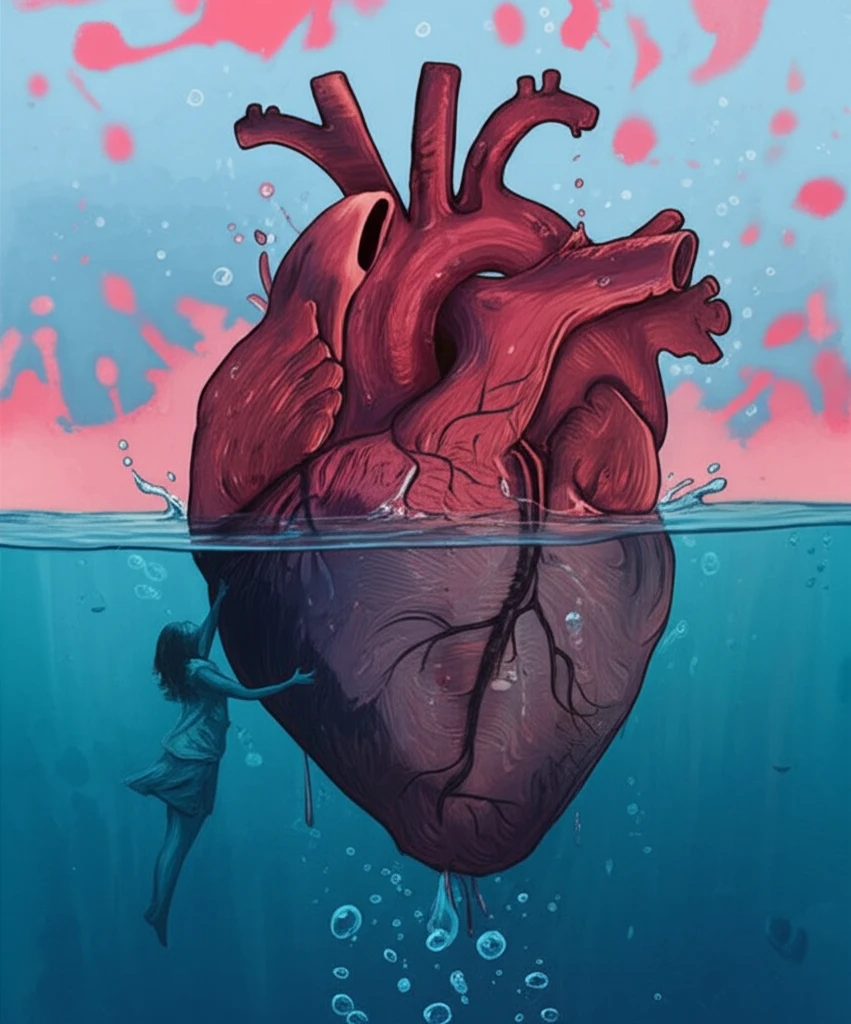
Think of your heart as a super-efficient pump. In AHF, this pump falters. This can happen because of a sudden weakening of the heart muscle, stiffening of the heart chambers, or an overwhelming increase in the body's demand for blood. Several factors contribute to this pump malfunction:
- Pulmonary Edema: Fluid leaks into the lungs, causing shortness of breath and difficulty breathing.
- Chamber Stiffness: The heart muscle becomes stiff, making it harder for the heart to fill with blood.
- Reduced Pump Performance: The heart muscle weakens and can't pump blood effectively.
Take Charge of Your Heart Health Today!
Acute heart failure is a serious condition, but knowledge is power. By understanding your risk factors, recognizing the symptoms, and seeking prompt medical attention, you can protect your heart and live a longer, healthier life. Don't wait for a crisis – make heart health a priority today!
