Decoding Superbugs: Your Guide to Fighting Multidrug-Resistant Infections
"Understanding MRSA and VRE: Effective Strategies for Battling Antibiotic-Resistant Bacteria"
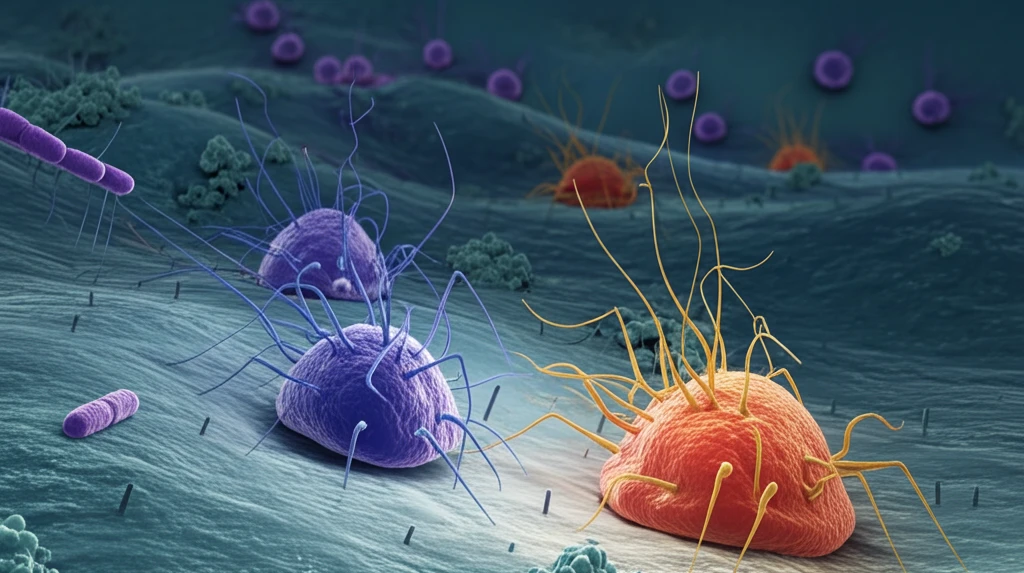
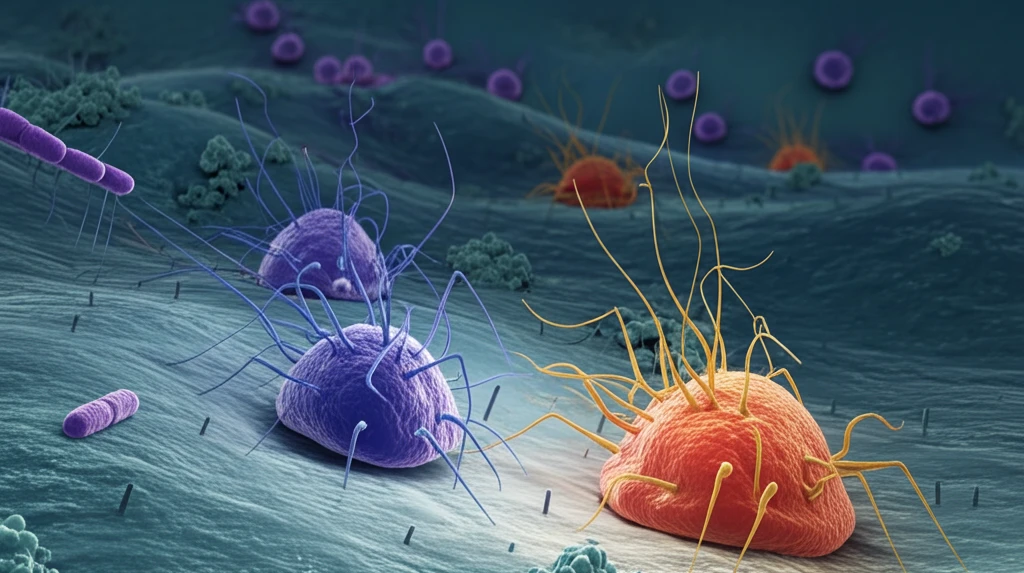
In today's world of medicine, multidrug-resistant (MDR) strains of bacteria are posing a significant challenge. When bacteria become resistant to multiple antibiotics, infections become harder to treat, leading to prolonged illness, higher healthcare costs, and increased mortality. It's crucial to understand these 'superbugs' to protect ourselves and our communities.
MDR bacteria are broadly defined as those resistant to at least three different classes of antibiotics. The most common method to identify these bacteria involves testing their in vitro resistance to key antimicrobial agents. This process leads to the creation of acronyms like VRE (vancomycin-resistant Enterococcus) or MRSA (methicillin-resistant Staphylococcus aureus), helping healthcare professionals quickly recognize and address these threats.
The Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO) have highlighted the urgent need to address antibiotic resistance. These organizations have identified priority lists of antibiotic-resistant bacteria to guide research and the development of new, effective drugs. In this article, we’ll explore the treatment of bloodstream infections (BSIs) caused by two high-priority MDR Gram-positive pathogens: MRSA and VRE.
Current Treatment Options
While glycopeptides like vancomycin (VAN) are often the first line of defense against MRSA infections, their effectiveness has been increasingly questioned. Several factors contribute to this, including limited tissue distribution, slow bactericidal activity, and high protein binding. This has led to a higher prevalence of treatment failure with glycopeptides in severe MRSA infections. Additionally, there’s debate about the impact of VAN mean minimal inhibitory concentrations (MIC) creep, which refers to the progressive increase in the mean MIC of VAN in clinical isolates.
- Vancomycin (VAN): Often the first line, but effectiveness is questioned due to factors like limited tissue distribution.
- Linezolid (LND): Used for skin and lower respiratory tract infections; bacteriostatic properties raise concerns for MRSA bacteremia.
- Tedizolid (TED): Newer option for skin infections, but lacks data for MRSA and VRE bloodstream infections.
- Daptomycin (DAP): Effective against MDR Gram-positive pathogens, but resistance remains a concern; higher doses may be needed.
Expert Opinion and Recommendations
Managing MRSA and VRE bloodstream infections requires a careful and strategic approach. While vancomycin remains a common starting point, it's essential to consider alternatives like linezolid or daptomycin, especially in cases of reduced vancomycin susceptibility or specific patient conditions. The combination of daptomycin with beta-lactam antibiotics shows promise, particularly for preventing resistance. Staying informed about emerging resistance patterns and treatment options is key to combating these challenging infections effectively.
