Decoding Myositis: A Practical Guide to Spotting and Managing Muscle Inflammation
"Early suspicion and comprehensive management are key to navigating the complexities of myositis, a group of inflammatory muscle diseases."
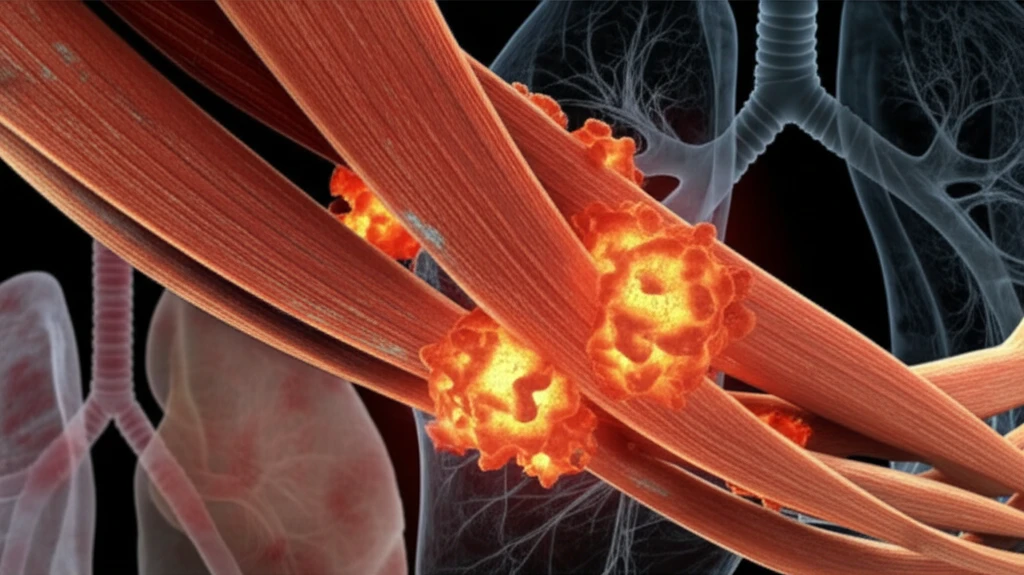
Myositis refers to a group of inflammatory conditions affecting the skeletal muscles. While all myositis share muscle inflammation as a core feature, the severity and impact can vary greatly, ranging from subtle, asymptomatic cases to severe, debilitating muscle weakness. Adding to the complexity, myositis often presents as part of a systemic illness, affecting multiple organs beyond just the muscles.
This widespread impact makes early detection and accurate diagnosis critical. Recognizing the signs, understanding the diagnostic pathways, and implementing appropriate management strategies are key to improving outcomes for individuals with myositis. The good news is that advances in identifying specific auto-antibodies have significantly improved diagnosis and classification, though muscle biopsy remains essential in many cases.
This article provides a practical guide to understanding myositis, drawing on the latest research to explain how to suspect, confirm, and manage the condition. We'll explore the key signs and symptoms, diagnostic tools, and management strategies to empower you with the knowledge you need.
When to Suspect Myositis: Recognizing the Clues
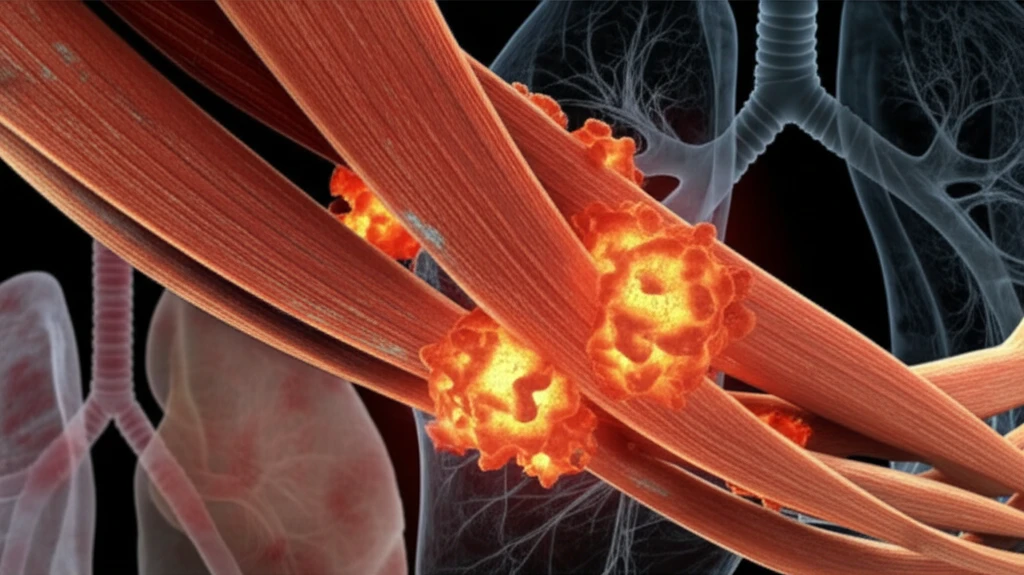
Because myositis can manifest in diverse ways, vigilance is key. Suspect myositis when encountering certain clinical scenarios, especially those involving muscle-related symptoms, skin manifestations, lung involvement, or joint issues. Let's break down specific signs that should raise suspicion:
- Difficulty rising from a seated position (sign of the stool).
- Using hands to push oneself up from the floor (Gowers' sign).
- Inability to hold limbs elevated against gravity (Barré sign).
Empowering Outcomes: A Summary of Key Actions
Myositis presents a complex diagnostic and management challenge, but heightened awareness and strategic action can significantly improve patient outcomes. By maintaining a high index of suspicion in relevant clinical scenarios, clinicians can leverage auto-antibody testing and muscle biopsies to confirm the diagnosis and classify the specific myositis subtype.
Remember that optimal management extends beyond addressing muscle inflammation. Vigilant monitoring and proactive management of systemic complications (pulmonary, cardiac, gastrointestinal, and joint involvement) and co-morbidities (cancer risk, cardiovascular risk, thromboembolic risk, fracture risk) are equally critical for improving the long-term prognosis.
While randomized controlled trials in myositis are limited, a range of medications are available. Expert guidance is essential to tailor treatment strategies and optimize the use of available therapies to meet individual patient needs.
