Decoding Gum Disease: Understanding Aggressive Periodontitis and Its Impact
"A deep dive into the clinical and microbiological factors behind generalized aggressive periodontitis and how it affects young adults."
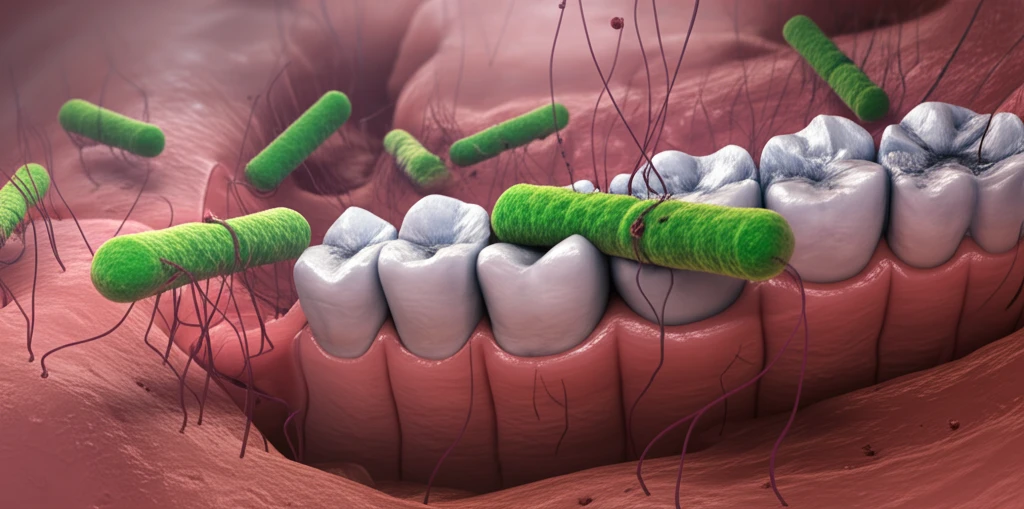
Periodontitis, commonly known as gum disease, is characterized by inflammation and the breakdown of tissues supporting the teeth. This condition arises from an imbalance between subgingival microorganisms and the host's immune response. The two main types of periodontitis are chronic and aggressive, with aggressive periodontitis (PAg) being less prevalent but posing a significant risk.
Aggressive periodontitis (PAg) is notable for its rapid progression and marked loss of attachment, often leading to early tooth loss and significant alveolar damage. Understanding this condition is crucial because, despite its lower occurrence, its impact on oral health can be severe.
PAg is defined by its rapid advancement, primarily affecting young, systemically healthy individuals. Clinically, it's classified as localized when it affects first molars and incisors, or generalized when it involves at least three permanent teeth beyond these. A key clinical feature is the severe periodontal destruction relative to the amount of bacterial deposits.
Clinical and Microbiological Characteristics of Aggressive Periodontitis
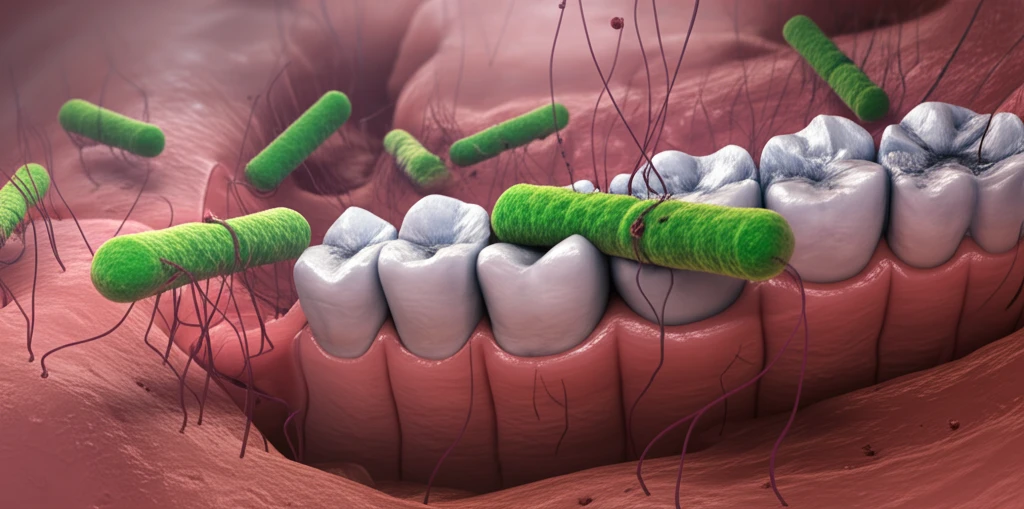
A recent study delved into the clinical and microbiological characteristics of patients diagnosed with generalized aggressive periodontitis (PAgG). Conducted at the dental clinics of the University of Antioquia in Medellín, Colombia, the cross-sectional study involved 20 participants under 30 years of age. Microbiological samples were analyzed using culture techniques, taken from the deepest sites (≥ 5mm) in each patient's mouth.
- Large proportions of Prevotella spp and F. nucleatum.
- Porphyromonas gingivalis found in half the participants.
- 10% tested positive for gram-negative enteric bacilli.
Implications and Future Directions
Understanding the microbial flora in PAgG is essential for selecting appropriate antibiotic therapies. The study suggests that antimicrobials like azithromycin or doxycycline, which have limited effects on subgingival flora, may not be suitable. Instead, therapies involving amoxicillin and metronidazole, or moxifloxacin, show promise in managing PAgG.
