Cell Docking: A Revolutionary Approach to Stroke Treatment
"New research reveals a high-throughput analysis of cell docking to the vessel wall, potentially transforming intra-arterial cell targeting and neuroinflammation studies. Explore how ITGA4-engineered cells are paving the way for stroke breakthroughs."
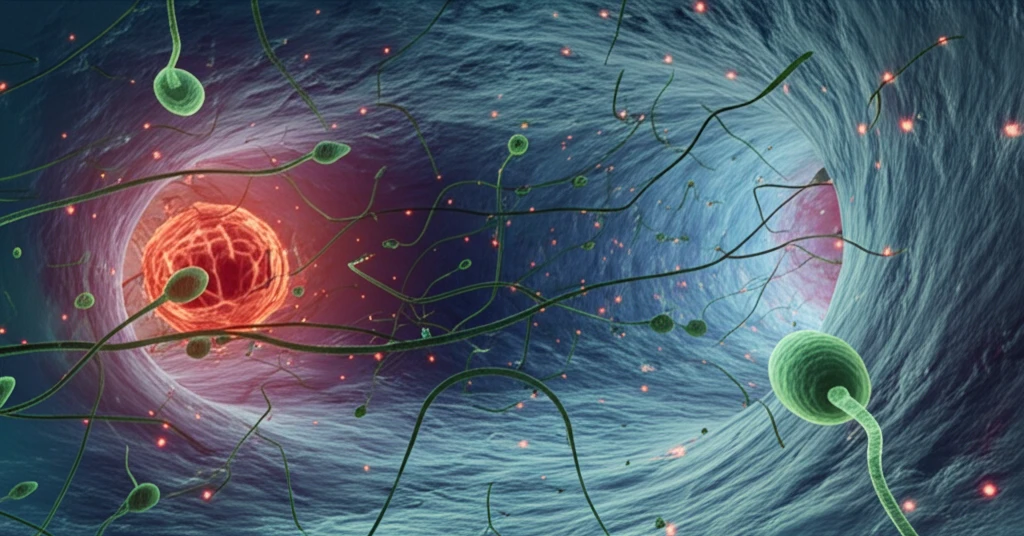
Stroke remains a leading cause of disability, spurring relentless research into more effective treatments. Mesenchymal stem cells (MSCs) have shown promise in animal models, primarily through immunomodulation and paracrine activity. However, delivering these cells intravenously requires high quantities, posing feasibility challenges for human applications. A more direct approach involves intra-arterial delivery, which routes cells directly to the brain, thus reducing the necessary dosage.
Recent advancements focus on enhancing cell homing through cell engineering, further optimizing the intra-arterial route. This is where innovative microfluidic platforms come into play, enabling the screening and selection of molecules that improve the docking of stem cells to the vessel wall. Imagine a future where targeted cell therapies dramatically improve stroke outcomes. This is now more conceivable than ever.
This article will delve into a groundbreaking study that developed a microfluidic platform to analyze cell docking. The study highlights the potential of ITGA4-engineered MSCs to improve cell homing to the brain, offering new avenues for treating stroke and other neuroinflammatory conditions. The insights from this research could significantly alter how we approach cell-based therapies in the future.
Decoding the Cell Docking Mechanism
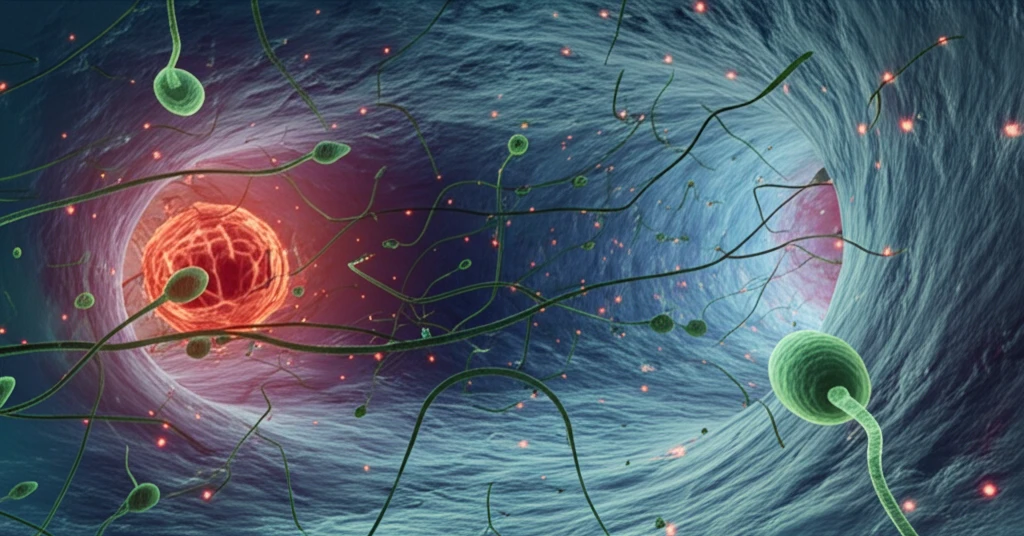
The core of this innovative approach lies in understanding and manipulating the cell docking mechanism. Researchers engineered MSCs to overexpress ITGA4, an adhesion molecule crucial for cell interaction with the vessel wall. The process involved using mRNA-based transfection, a sophisticated method allowing for enhanced control over protein expression in MSCs. This technique bypasses challenges associated with traditional DNA plasmid-based methods, providing a more efficient way to modify cell behavior.
- ITGA4 Overexpression: Enhances cell adhesion to the vessel wall.
- Microfluidic Platform: Provides a controlled environment mimicking activated blood vessels.
- MIRB Tagging: Enables precise tracking and analysis of cell behavior.
The Future of Targeted Cell Therapies
This research signifies a major stride toward more targeted and effective stroke therapies. By developing a robust platform for analyzing cell docking and validating the potential of ITGA4-engineered MSCs, the study paves the way for future investigations into other adhesion molecules and cell engineering strategies. The ultimate goal is to refine cell-based therapies to maximize their impact on stroke recovery and other neuroinflammatory conditions.
