Bladder Cancer Breakthrough: Is Intravesical Therapy a Game Changer?
"Examining the Latest Research on Intravesical Bacillus Calmette-Guérin (BCG) and Chemohyperthermia (C-HT) for High-Risk Bladder Cancer Patients."
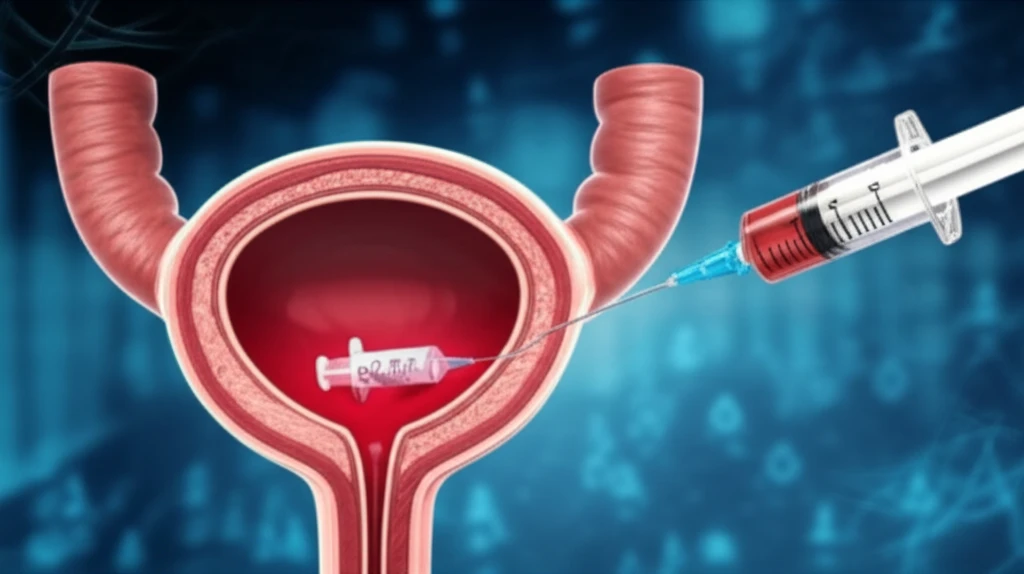
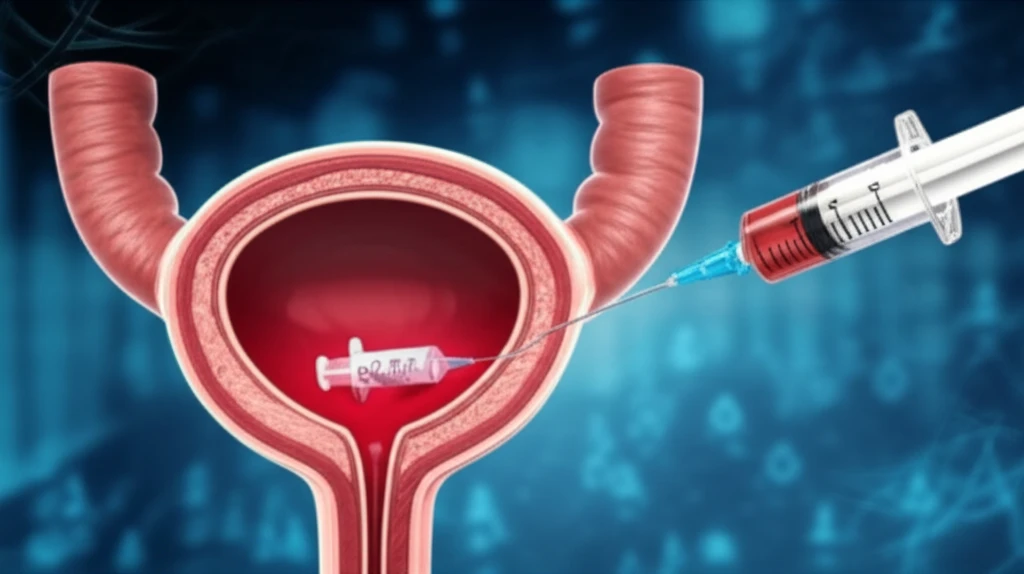
Bladder cancer, while often treatable, remains a significant health concern, with over 75% of cases classified as non-muscle-invasive bladder cancer (NMIBC) at diagnosis. For individuals diagnosed with high-risk NMIBC, the journey towards recovery involves aggressive treatment to prevent recurrence and disease progression. Adjuvant intravesical therapy, which involves administering medication directly into the bladder, is a critical part of the treatment plan.
Among these therapies, intravesical bacillus Calmette-Guérin (BCG) has long been a frontline option. However, its effectiveness is sometimes counterbalanced by side effects, and the search for alternative or improved treatments continues. Chemohyperthermia (C-HT), which combines chemotherapy with heat, has emerged as another promising approach. Recent research has focused on directly comparing the efficacy of BCG and C-HT, offering new insights into which treatment might offer better outcomes for patients.
This article delves into a recent study comparing BCG and chemohyperthermia, focusing on recurrence-free intervals and the overall effectiveness of these treatments. By examining the data and findings, we will provide a clearer understanding of the current landscape of bladder cancer treatment, including what the research shows about the best treatment options for high-risk patients.
BCG vs. Chemohyperthermia: What the Research Reveals
The study, published in the Canadian Urological Association Journal in 2015, examined a cohort of patients who underwent treatment for bladder cancer between January 2004 and January 2014. The researchers analyzed data from patients who received intravesical treatments. The aim of the study was to evaluate the effectiveness of BCG and C-HT in managing high-risk NMIBC, particularly focusing on recurrence-free intervals and the prevention of disease progression. The study used a propensity score-matched analysis to compare the outcomes of patients treated with each therapy, with the goal of minimizing bias and ensuring a fair comparison.
- Recurrence-Free Interval: BCG treatment demonstrated a significantly longer recurrence-free interval compared to C-HT.
- Tumor Recurrence Risk: C-HT was associated with a higher risk of tumor recurrence.
- Disease Progression: There was no significant difference in the progression rates between the two treatments.
Looking Ahead: Advancements and Future Directions
The study's conclusions highlight the ongoing evolution of bladder cancer treatment. While BCG remains a cornerstone, research is continuously seeking improvements and alternatives, especially for patients who may not respond well to BCG or experience significant side effects. C-HT shows promise in some cases, but it is not as effective as BCG. As the medical field progresses, the focus remains on enhancing treatment efficacy, minimizing side effects, and improving the long-term outcomes for individuals facing bladder cancer. Ongoing research and clinical trials will continue to refine treatment strategies, bringing renewed hope and improved quality of life for patients.
