Beyond Surgery: How Minimally Invasive Techniques Are Revolutionizing Abdominal Care
"Explore the groundbreaking world of endoscopic ultrasound (EUS) and its impact on treating complex abdominal conditions with less pain and faster recovery."
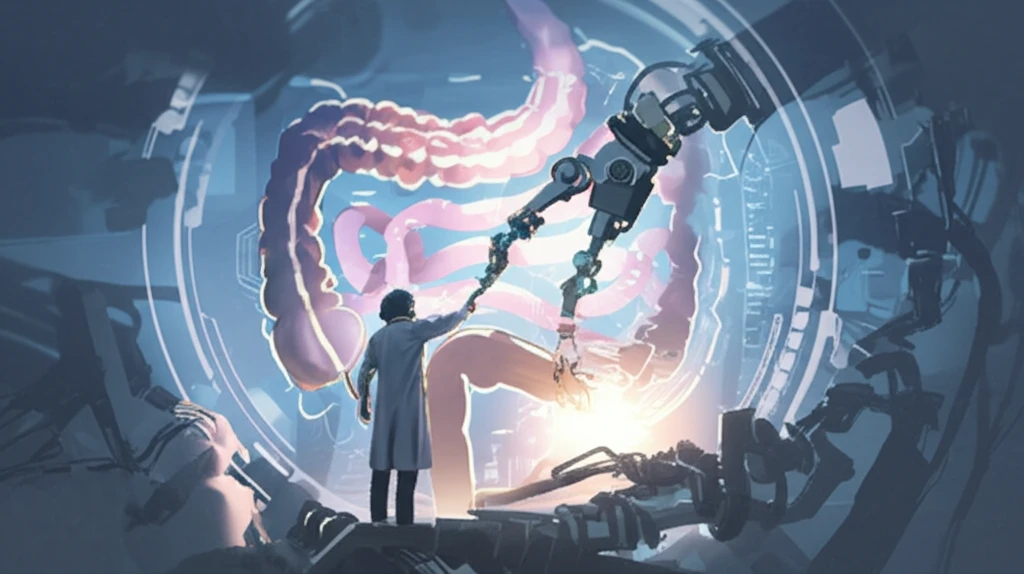
For years, traditional surgery was the primary approach to addressing complex abdominal conditions, often involving lengthy hospital stays and significant recovery periods. However, the landscape of abdominal care is undergoing a dramatic shift, thanks to the rise of minimally invasive techniques. Among these, endoscopic ultrasound (EUS) stands out as a revolutionary tool, offering a less invasive alternative to traditional surgery for a wide range of conditions.
Endoscopic ultrasound is not just another medical procedure; it's a paradigm shift in how we approach abdominal and pelvic health. By combining endoscopy and ultrasound technologies, EUS allows doctors to visualize and access areas previously reachable only through open surgery. This means smaller incisions, reduced pain, shorter hospital stays, and faster recovery times for patients.
This article explores the exciting world of EUS, focusing on its applications in creating anastomoses (connections) within the digestive system, draining fluid collections in the abdomen and pelvis, and performing vascular interventions. As we delve into the details, you'll discover how these minimally invasive techniques are providing new hope and improved outcomes for patients facing complex medical challenges.
EUS-Guided Anastomosis: A New Path for Digestive Health
Gastric outlet obstruction (GOO), a condition where the passage of food from the stomach is blocked, has traditionally been treated with open or laparoscopic surgery. However, EUS offers a less invasive way to create a connection between the stomach and the small intestine, bypassing the obstruction. This procedure, known as EUS-guided gastroenterostomy (EUS-GE), is performed using a special endoscope equipped with an ultrasound probe.
- Minimally invasive approach
- Reduced risk of complications
- Shorter recovery time
- Improved quality of life
The Future of Abdominal Care: A Minimally Invasive Revolution
Endoscopic ultrasound is at the forefront of a revolution in abdominal care, offering less invasive solutions for complex medical problems. As technology advances and experience grows, EUS-guided procedures are poised to become even more widely adopted, transforming the lives of patients and reshaping the future of medicine. Embracing these innovative techniques promises a future where treatment is less invasive, recovery is faster, and outcomes are better than ever before.
