AngioJet Thrombectomy: Weighing the Risks of Kidney Injury in DVT Treatment
"A new study sheds light on the potential risks of acute kidney injury (AKI) associated with the AngioJet system compared to traditional methods for treating deep vein thrombosis."
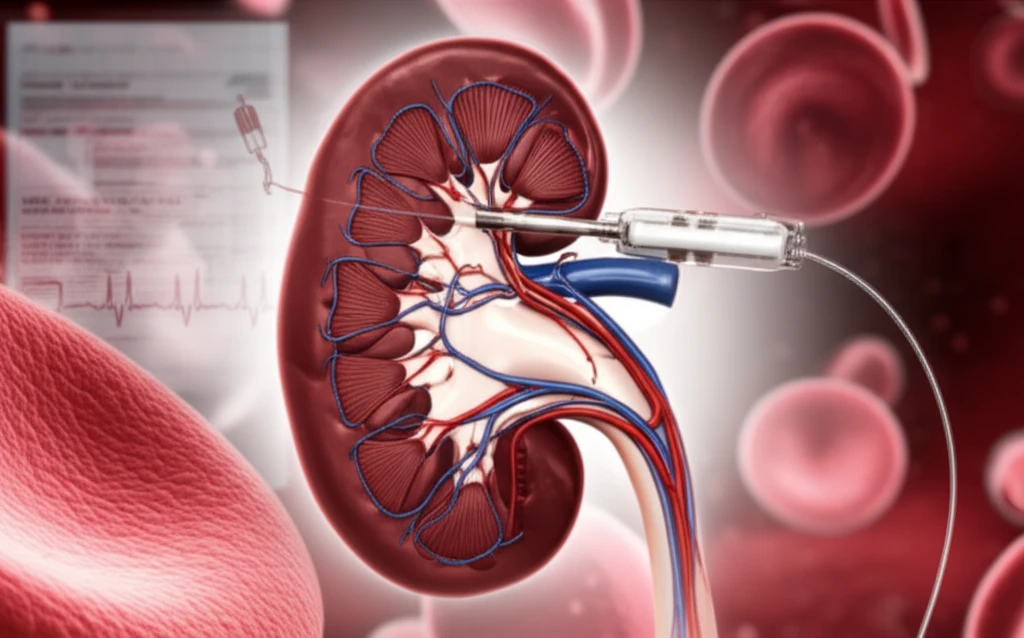
Deep vein thrombosis (DVT), particularly in the iliofemoral region, is a serious condition that can lead to long-term complications such as post-thrombotic syndrome. To minimize these risks, percutaneous mechanical thrombectomy (PMT) and catheter-directed thrombolysis (CDT) are often employed to remove the blood clot and restore proper blood flow.
Among the PMT devices, the AngioJet system has gained popularity due to its ability to rapidly break down and remove clots. However, a recent study has raised concerns about a potential side effect: an increased risk of acute kidney injury (AKI) following the procedure.
This article delves into the findings of this study, comparing the risk of AKI between AngioJet PMT and CDT, and explores the factors that may contribute to this increased risk. Understanding these nuances is crucial for patients and healthcare providers alike in making informed decisions about DVT treatment.
AngioJet vs. CDT: Understanding the Kidney Injury Risk
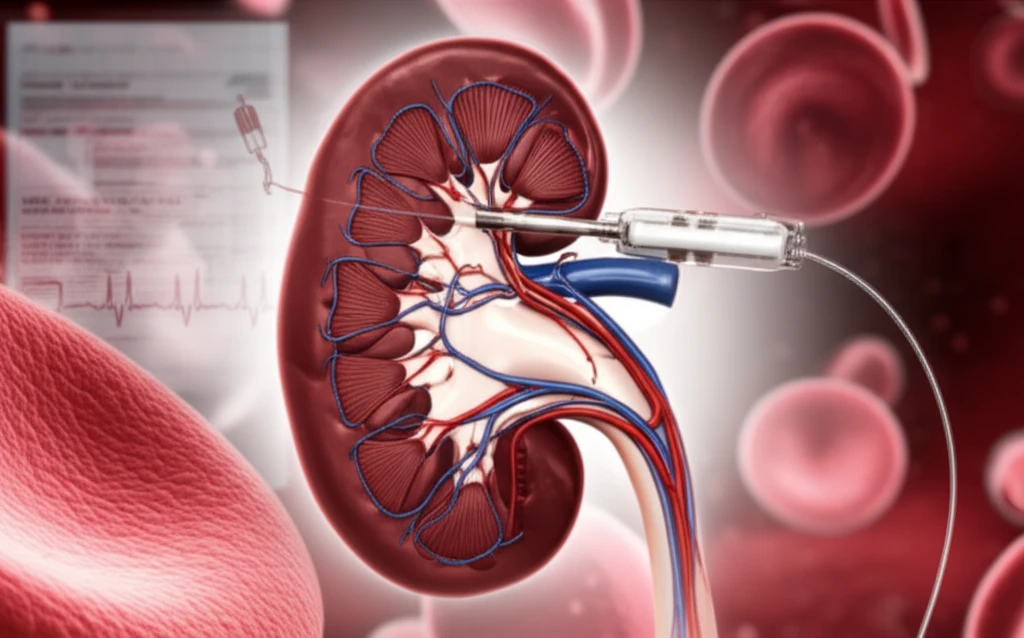
The study, published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders, retrospectively examined the medical records of 198 patients with acute iliofemoral DVT. These patients underwent either AngioJet PMT or CDT between January 2014 and September 2017. The researchers then compared the incidence of postoperative AKI between the two groups.
- Use of AngioJet PMT (odds ratio [OR], 2.82)
- History of major surgery within 3 months of endovascular intervention (OR, 8.51)
- Hematocrit (HCT) drop >14% (OR, 2.73)
Making Informed Decisions About DVT Treatment
The study highlights the importance of carefully weighing the risks and benefits of different DVT treatment options, especially considering individual patient factors. While AngioJet PMT can be a valuable tool for rapid clot removal, healthcare providers should be aware of the increased risk of AKI, particularly in patients with recent surgical history or those prone to significant hematocrit drops. By understanding these risks and taking appropriate precautions, clinicians can optimize patient outcomes and minimize potential complications.
